Outpatient Substance Abuse Rehabilitation Treatment Plan Form Page 2
ADVERTISEMENT
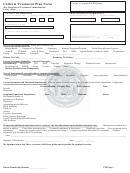
Outpatient Substance Abuse Rehabilitation Treatment Plan Form
Mailing Address: Behavioral Health Department, 48 Monroe Turnpike Trumbull, CT 06611 Phone: 1-800-201-6991 Fax: 1-800-760-4041
Section I. Member and Provider Information
Treating provider: ______________________________________________
Provider ID #: ________________________________
Provider phone number: ________________________
Provider fax number: ____________________________
Member ID #: ________________________________
Reference #:__________________________________
Member initials: ______________
Date of evaluation: ____/____/____
Member age: ______
Date of first session: ____/____/____
Number of sessions since start of treatment: ______________
K
K
K
K
Has Member given approval to contact his/her PCP?
Yes
No
Have you contacted the Member’s PCP?
Yes
No
Section VII. Response to Treatment
K
K
1. Has the patient attended a treatment program on a regular basis?
Yes
No
K
K
2. Has the patient attended a 12-step or other program on a regular basis?
Yes
No
If no to either of the above, why? ________________________________________________________________________________
__________________________________________________________________________________________________________
K
K
If so, do they have a home group and sponsor?
Yes
No
K
K
3. Is there family involvement?
Yes
No
If so, who and to what extent? __________________________________________________________________________________
If no, why? ________________________________________________________________________________________________
K
K
4. Has the patient relapsed?
Yes
No
If so, when? ______________________
How has the treatment plan changed to address the relapse?________________________
__________________________________________________________________________________________________________
5. How is the potential for relapse addressed in the treatment plan? __________________________________________________________
__________________________________________________________________________________________________________
K
K
6. Is the patient on psychiatric medications?
Yes
No
If so, please describe current medications and response to treatment. ______________________________________________________
__________________________________________________________________________________________________________
K
K
Who is prescribing medications?
PCP
Psychiatrist: ________________________
Name
7. List other changes in: treatment plan/patient’s response/diagnosis. ________________________________________________________
__________________________________________________________________________________________________________
8. What is the discharge plan? ____________________________________________________________________________________
__________________________________________________________________________________________________________
9. What is the estimated length of treatment?__________________________________________________________________________
10. How many additional visits are being requested? ____________________________________________________________________
Provider signature: ________________________________________________________
Date: ____________________________
For Insurer Use Only: ____ additional sessions have been certified from ___ /___ /___ to ___ /___ /___ by the Behavioral Health
Department. A total of _____ sessions (including prior sessions) have been authorized by. Note: All certifications are based upon
Member eligibility and benefit availability at the time services are rendered.
MS-03-404
page 2 of 2
2927 R3
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1 2
2