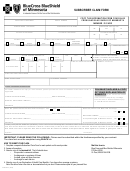
Anthem Subscriber Submitted Claim Form Page 2
ADVERTISEMENT
SUBSCRIBER CLAIM FILING INFORMATION (HOW TO FILE)
Be sure to ask your provider of care if he/she bills a statement to Anthem Blue Cross and Blue Shield. Please submit
statements only if the provider does not bill us directly. To receive benefits for RX, or for services by a provider who does
not bill us directly, complete the claim form, attach itemized bills, and mail the white copy to Anthem Blue Cross and Blue
Shield, P.O. Box 17849, Denver, Colorado 80217-0849.
Keep a duplicate copy of your itemized bills as they will not be returned to you. This claim may be returned to you if all
required information is not present.
CLAIM FILING INSTRUCTIONS
(Corresponds to numbered items on claim form)
A separate claim form for each family member and each provider of care must be submitted.
ITEM NO.
1–8 Please complete all blocks. all fields required.
14 Statement of why these services were required.
16 Indicate the name of the physician, pharmacy, hospital or other institutional facility who has billed for services
provided to the patient. Only one provider per form (however, multiple pharmacy bills may be attached to
one claim form.)
17 If laboratory or radiology services are being billed by a professional provider, and the place of service was
inpatient or outpatient hospital, indicate the name of the hospital.
18 Name and telephone number; whoever can help us if additional information is required.
19 Use a separate line for each date of service and receipt.
20 Write the appropriate code to indicate the place of service by using the legend below this section.
21 Indicate the total charge for each service.
22 Briefly indicate the type of service, i.e. lab, X-ray, surgery, therapy, cast, stitches, etc.
23 This amount represents the total of all charges to be considered for benefit.
24 Your signature attests to the accuracy and completeness of all information on the claim and the attachments
and authorizes the release of your medical records by the provider to our office if necessary.
REQUIRED INFORMATION
Itemized Bills: Summarizing the services may help us better understand the attachments if they are not clear. The
attached itemized bills must include the provider name, patient’s name, date of service, detailed description of service,
and amount charged for that service. These must be valid documents from the provider.
Psychotherapy: Length and type of session (group or individual). Name and professional status of the individual con-
ducting the session.
Prescription Drugs: Patient’s name, pharmacy name and address, purchase date, drug name, prescription number and
charge. The bill or receipt must be issued by the pharmacy.
HELPFUL HINTS
•
If you have questions or need assistance, contact Anthem Blue Cross and Blue Shield Customer Service.
•
To reduce the possibility of small billings getting lost or separated, it would be helpful if you attach these to an 8 1/2x11 piece of paper.
•
We encourage you to file claims within 90 days of the service date. Please refer to your Benefit Certificate for specific timely filing limitations.
•
File only if the provider has not.
Important: If the services for this claim were provided by a participating physician or hospital, the benefit payment will go to the provider. However, if
you paid this participating provider in full, attach a copy or your cancelled check or receipt and we will direct the benefit payment to you. Indicate “PAID
IN FULL” under item 24.
A complete description of your benefits, as well as limitations and exclusions applicable thereto, is available in the Benefit Certificate. Final
interpretation of any and all provisions of the program is governed by the Benefit Certificate.
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Business
 1
1 2
2