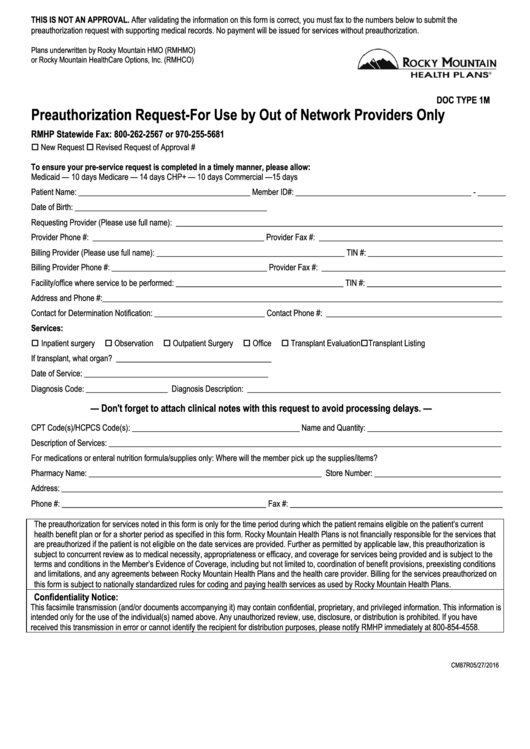
Preauthorization Request Form - For Use By Out Of Network Providers Only
ADVERTISEMENT
THIS IS NOT AN APPROVAL. After validating the information on this form is correct, you must fax to the numbers below to submit the
preauthorization request with supporting medical records. No payment will be issued for services without preauthorization.
Plans underwritten by Rocky Mountain HMO (RMHMO)
or Rocky Mountain HealthCare Options, Inc. (RMHCO)
DOC TYPE 1M
Preauthorization Request-For Use by Out of Network Providers Only
RMHP Statewide Fax: 800-262-2567 or 970-255-5681
New Request
Revised Request of Approval #
To ensure your pre-service request is completed in a timely manner, please allow:
Medicaid — 10 days
Medicare — 14 days
CHP+ — 10 days
Commercial —15 days
Patient Name: __________________________________________ Member ID#: ___________________________________________ - _______
Date of Birth: _______________________________________________
Requesting Provider (Please use full name): ________________________________________________________________________________
Provider Phone #: __________________________________________ Provider Fax #: _____________________________________________
Billing Provider (Please use full name): ______________________________________________ TIN #: _________________________________
Billing Provider Phone #: ______________________________________ Provider Fax #: _____________________________________________
Facility/office where service to be performed: _________________________________________ TIN #: _________________________________
Address and Phone #:__________________________________________________________________________________________________
Contact for Determination Notification: ___________________________ Contact Phone #: ___________________________________________
Services:
Inpatient surgery
Observation
Outpatient Surgery
Office
Transplant Evaluation
Transplant Listing
If transplant, what organ? ______________________________________
Date of Service: _____________________________________________
Diagnosis Code: ____________________ Diagnosis Description: ______________________________________________________________
— Don't forget to attach clinical notes with this request to avoid processing delays. —
CPT Code(s)/HCPCS Code(s): _________________________________________ Name and Quantity: _________________________________
Description of Services: ________________________________________________________________________________________________
For medications or enteral nutrition formula/supplies only: Where will the member pick up the supplies/items?
Pharmacy Name: _________________________________________________________ Store Number: _______________________________
Address: ____________________________________________________________________________________________________________
Phone #: __________________________________________________ Fax #: ____________________________________________________
The preauthorization for services noted in this form is only for the time period during which the patient remains eligible on the patient’s current
health benefit plan or for a shorter period as specified in this form. Rocky Mountain Health Plans is not financially responsible for the services that
are preauthorized if the patient is not eligible on the date services are provided. Further as permitted by applicable law, this preauthorization is
subject to concurrent review as to medical necessity, appropriateness or efficacy, and coverage for services being provided and is subject to the
terms and conditions in the Member’s Evidence of Coverage, including but not limited to, coordination of benefit provisions, preexistin g conditions
and limitations, and any agreements between Rocky Mountain Health Plans and the health care provider. Billing for the services preauthorized on
this form is subject to nationally standardized rules for coding and paying health services as used by Rocky Mountain Health Plans.
Confidentiality Notice:
This facsimile transmission (and/or documents accompanying it) may contain confidential, proprietary, and privileged information. This information is
intended only for the use of the individual(s) named above. Any unauthorized review, use, disclosure, or distribution is proh ibited. If you have
received this transmission in error or cannot identify the recipient for distribution purposes, please notify RMHP immediately at 800-854-4558.
CM87R05/27/2016
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1