Medical Member Claim Form - Blue Cross - California Page 2
ADVERTISEMENT
HOW TO USE THIS FORM
Dear Member:
Usually, all providers of health care will bill us for services to you and your enrolled dependents. This is the preferred procedure. You are not
bothered with claim forms and we often need more details than are ordinarily provided on bills to patients.
Sometimes, a physician may not bill us or an ambulance company, for example, may send the bill directly to you. In either instance, we have
no way of knowing about your claim. This Member Claim Form was developed to notify us of any covered health service for which we have not
already been billed. Please read the following instructions about how to report Health Care Services.
We are happy to serve you.
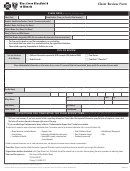
PATIENT INFORMATION
SUBSCRIBER INFORMATION (on member ID card)
Use this section to identify the patient and subscriber. Some of this information may be found on your member ID card.
MEDICAL INFORMATION
HEALTH CARE SERVICES: Use this section to report any COVERED health service which has not already been reported to this
Anthem Blue Cross Plan by the provider of service (the physician, clinical, ambulance company, private duty nurse, etc.) Attach an itemized bill
or photocopy. Please be sure that duplicate bills are not submitted.
DATE OF SERVICE
PROVIDER OF SERVICE
SERVICE RENDERED
ILLNESS OR DIAGNOSIS
TOTAL
(Mo/Day/Yr)
(Name of Doctor, Lab, Amb. Co., etc.)
(Office Visit, X-ray, etc.)
7/9/07
John Wang, M.D.
Office Visit
Bronchitis
$35.00
7/9/07
Pat Fogarty, M.D.
X-ray
Strain
$57.00
$92.00
GRAND TOTAL
THE FOLLOWING INFORMATION MUST ALSO BE INCLUDED ON BILLS FOR THESE ITEMS:
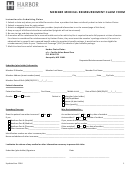
REGISTERED AND LICENSED VOCATIONAL NURSES:
• Hours and dates of service
• Location of service (residence or name of hospital)
• Written documentation of physician’s referral (must include the state license number, plan of treatment and estimated duration
of treatments)
PROSTHETIC DEVICES, APPLIANCES OR DURABLE MEDICAL EQUIPMENT:
• Doctor’s orders or prescription
• Purchase price
AMBULANCE
• Pick-up and delivery points
• Number of miles
BILLS MUST BE ITEMIZED
Cancelled checks, cash register receipts and non-itemized “balance due” statements cannot be processed. Each itemized bill must include:
• Name and address of provider (doctor, hospital, laboratory, ambulance service, etc.)
• Name of patient
• Service provided
• Date of service
• Amount charged for each service
• Diagnosis
CLAIM MAILING INSTRUCTIONS:
For services rendered in California, please send claims to Anthem Blue Cross, P.O. Box 60007, Los Angeles, CA 90060.
For non-California services, please contact Customer Service for the claims office address. Mail claims to the Blue Cross and/or Blue Shield
Plan of the state in which services were rendered. For your convenience the Customer Service number is listed on your Member ID card.
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Business
 1
1 2
2