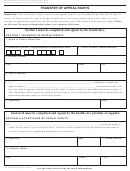
Form Cms-701 - Updated Plan Of Progress For Outpatient Rehabilitation Page 2
ADVERTISEMENT
INSTRUCTIONS FOR COMPLETION OF FORM CMS-701
(Enter dates as 6 digits, month, day, year)
14. Recertification - Enter the inclusive dates when recertification
1. Patient’s Name - Enter the patient’s last name, first name and
is required, even if the ON FILE box is checked in item 17.
middle initial as shown on the health insurance Medicare card.
Check the N/A box if recertification is not required for the type
2. Provider Number - Enter the number issued by Medicare to
of service rendered.
the billing provider (i.e., 00–7000).
15. Physician’s Signature - If the form CMS-701 is used for
3. HICN - Enter the patient’s health insurance number as shown
recertification, the physician enters his/her signature. If
on the health insurance Medicare card, certification award,
recertification is not required for the type of service rendered,
utilization notice, temporary eligibility notice, or as reported
check N/A box. If the form CMS-701 is not being used for
by SSO.
recertification, check the ON FILE box - item 17. If discharge
is ordered, check DC box.
4. Provider Name - Enter the name of the Medicare billing
provider.
16. Date - Enter the date of the physician’s signature only if the
form is used for recertification.
5. Medical Record No. - (optional) Enter the patient’s medical/
clinical record number used by the billing provider. (This is an
17. On File (Means certification signature and date) - Enter the
item which you may enter for your own records.)
typed/printed name of the physician who certified the plan of
treatment that is on file at the billing provider. If recertification is
6. Onset Date - Enter the date of onset for the patient’s primary
not required for the type of service checked in item 8, type/print
medical diagnosis, if it is a new diagnosis, or the date of the
the name of the physician who referred or ordered the service,
most recent exacerbation of a previous diagnosis. If the exact
but do not check the ON FILE box.
date is not known enter 01 for the day (i.e., 120191). The date
matches occurrence code 11 on the UB-92.
18. Reason(s) For Continuing Treatment This Billing Period -
Enter the major reasons why the patient needs to continue
7. SOC (start of care) Date - Enter the date services began at
skilled rehabilitation for this billing period (e.g., briefly state
the billing provider (the date of the first Medicare billable visit
the patient’s need for specific functional improvement, skilled
which remains the same on subsequent claims until
training, reduction in complication or improvement in safety and
discharge or denial corresponds to occurrence code 35 for PT,
how long you believe this will take, if possible or state your
44 for OT, 45 for SLP and 46 for CR on the UB-92).
reasons for recommending discontinuance). Complete by the
rehab specialist prior to physician’s recertification.
8. Type - Check the type therapy billed; i.e., physical therapy
(PT), occupational therapy (OT), speech-language pathology
19. Signature - Enter the signature (or name) and the professional
(SLP), cardiac rehabilitation (CR), respiratory therapy (RT),
designation of the individual justifying or recommending need
psychological services (PS), skilled nursing services (SN), or
for care (or discontinuance) for this billing period.
social services (SW).
20. Date - Enter the date of the rehabilitation professional’s
9. Primary Diagnosis - Enter the pertinent written medical
signature.
diagnosis resulting in the therapy disorder and relating to 50%
or more of effort in the plan of treatment.
21. Check the box if services are continuing or discontinuing at end
of this billing period.
10. Treatment Diagnosis - Enter the written treatment diagnosis
for which services are rendered. For example, for PT the
22. Functional Level (end of billing period) - Enter the pertinent
primary medical diagnosis might be Degeneration of Cervical
progress made through the end of this billing period. Use
Intervertebral Disc while the PT treatment DX might be Frozen
objective terminology. Compare progress made to that shown
R Shoulder or, for SLP, while CVA might be the primary
on the previous CMS-701, item 22, or the CMS-700, items 20
medical DX, the treatment DX might be Aphasia.
and 21. Date progress when function can be consistently
If the same as the primary DX enter SAMPLE.
performed or when meaningful functional improvement is made
or when significant regression in function occurs. Your
11. Visits From Start of Care - Enter the cumulative total visits
intermediary reviews this progress compared to that on the
(sessions) completed since services were started at the billing
prior CMS-701 or 700 to determine coverage for this billing
provider for the diagnosis treated, through the last visit on this
period. Send a photocopy of the form covering the previous
bill. (Corresponds to UB-92 value code 50 for PT, 51 for OT,
billing period.
52 for SLP, or 53 for cardiac rehab.)
23. Service Dates - Enter the From and Through dates which
12. Current Frequency/Duration - Enter the current frequency
represent this billing period (should be monthly). Match the
and duration of your treatment; e.g., 3 times per week for 4
From and Through dates in field 6 on the UB-92. DO NOT use
weeks is entered 3/Wk x 4Wk.
00 in the date. Example: 01 08 91 for January 8, 1991.
13. Current Plan Update, Functional Goals - Enter the current
plan of treatment goals for the patient for this billing period. (If
the same as shown on the CMS-700 or previous 701 enter
“same”.) Enter the short-term goals to reach overall long-term
outcome. Justify intensity if appropriate. Estimate time-frames
to meet goals, when possible.
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1 2
2