Cobra Election Form - Calpers
ADVERTISEMENT
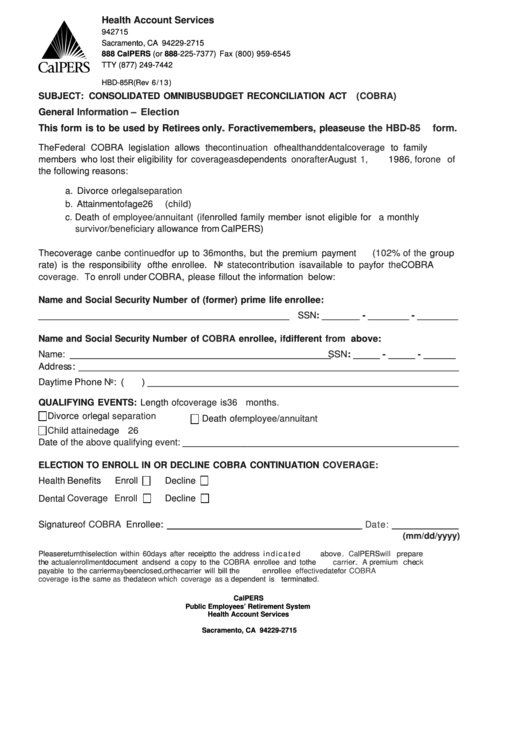
Health Account Services
1
P.O. Box 942715
Sacramento, CA 94229-2715
888 CalPERS (or 888-225-7377) Fax (800) 959-6545
TTY (877) 249-7442
HBD-85R (Rev 6/ 13)
SUBJECT: CONSOLIDATED OMNIBUS BUDGET RECONCILIATION ACT
(COBRA)
General
Information – Election
This form is to be used by Retirees
only.
For active members, please
use the HBD-85 form.
The Federal COBRA legislation allows the
continuation
of health
and dental coverage
to family
members who lost their eligibility for
coverage as
dependents
on
or
after
August
1, 1986,
for one of
the following reasons:
a. Divorce
or
legal
separation
b.
Attainment
of
age 26
(child)
c. Death
of employee/annuitant (if
enrolled family member is not eligible for
a
monthly
survivor/beneficiary
allowance from CalPERS)
The coverage
can
be
continued
for up to
36
months, but the premium payment
(102% of the
group
rate) is the responsibility of the enrollee. No
state
contribution is available to
pay
for
the
COBRA
coverage.
To enroll under
COBRA,
please fill out the information below:
Name and Social Security Number of (former) prime life enrollee:
_________________________________________________ SSN: _______ - ________ - ________
Name and Social Security Number of
COBRA
enrollee,
if
different
from
above:
Name: ___________________________________________________ SSN: _____ - _____ - ______
Address: _______________________________________________________________________________
Daytime Phone
No: (
) ______________________________________________________________
QUALIFYING EVENTS: Length
of coverage
is
36 months.
Divorce
or
legal
separation
Death of
employee/annuitant
Child attained
age
26
Date
of the above qualifying event: ______________________________________________________
ELECTION TO ENROLL IN OR DECLINE COBRA CONTINUATION
COVERAGE:
Health Benefits
Enroll
Decline
Dental
Coverage Enroll
Decline
Signature
of COBRA
Enrollee:
____________________________________
Date:
_____________
(mm/dd/yyyy)
Please return this
election within 60 days after
receipt
to the address i n d i c a t e d
above.
CalPERS
will
prepare
the
actual enrollment
document
and send a copy
to the
COBRA enrollee and to
the
carrier.
A premium
check
payable to
the
carrier
may
be enclosed, or the carrier will
bill
the enrollee
directly. The
effective
date for
COBRA
coverage is
the
same as
the date
on
which coverage as a
dependent is
terminated.
CalPERS
Public Employees’ Retirement System
Health Account Services
P.O. Box 942715
Sacramento, CA 94229-2715
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Legal
 1
1 2
2








