Form Cms-20014 - Notice Of Exclusions From Medicare Benefits - Skilled Nursing Facility (Nemb-Snf)
ADVERTISEMENT
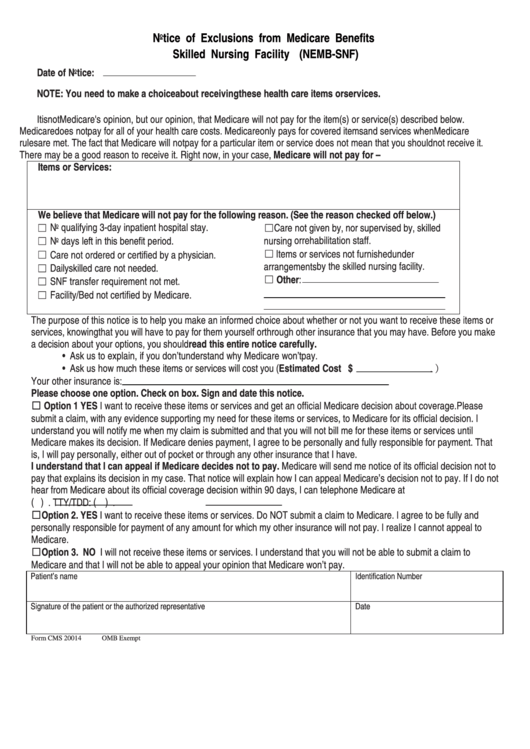
Notice of Exclusions from Medicare Benefits
Skilled Nursing Facility (NEMB-SNF)
Date of Notice:
NOTE: You need to make a choice about receiving these health care items or services.
It is not Medicare's opinion, but our opinion, that Medicare will not pay for the item(s) or service(s) described below.
Medicare does not pay for all of your health care costs. Medicare only pays for covered items and services when Medicare
rules are met. The fact that Medicare will not pay for a particular item or service does not mean that you should not receive it.
There may be a good reason to receive it. Right now, in your case, Medicare will not pay for –
Items or Services:
We believe that Medicare will not pay for the following reason. (See the reason checked off below.)
☐ No qualifying 3-day inpatient hospital stay.
☐Care not given by, nor supervised by, skilled
nursing or rehabilitation staff.
☐ No days left in this benefit period.
☐ Items or services not furnished under
☐ Care not ordered or certified by a physician.
arrangements by the skilled nursing facility.
☐ Daily skilled care not needed.
☐ Other:
☐ SNF transfer requirement not met.
☐ Facility/Bed not certified by Medicare.
The purpose of this notice is to help you make an informed choice about whether or not you want to receive these items or
services, knowing that you will have to pay for them yourself or through other insurance that you may have. Before you make
a decision about your options, you should read this entire notice carefully.
• Ask us to explain, if you don’t understand why Medicare won’t pay.
• Ask us how much these items or services will cost you (Estimated Cost $
.)
Your other insurance is:
Please choose one option. Check on box. Sign and date this notice.
☐ Option 1 YES I want to receive these items or services and get an official Medicare decision about coverage. Please
submit a claim, with any evidence supporting my need for these items or services, to Medicare for its official decision. I
understand you will notify me when my claim is submitted and that you will not bill me for these items or services until
Medicare makes its decision. If Medicare denies payment, I agree to be personally and fully responsible for payment. That
is, I will pay personally, either out of pocket or through any other insurance that I have.
I understand that I can appeal if Medicare decides not to pay. Medicare will send me notice of its official decision not to
pay that explains its decision in my case. That notice will explain how I can appeal Medicare’s decision not to pay. If I do not
hear from Medicare about its official coverage decision within 90 days, I can telephone Medicare at
(
)
. TTY/TDD: (
)
.
☐Option 2. YES I want to receive these items or services. Do NOT submit a claim to Medicare. I agree to be fully and
personally responsible for payment of any amount for which my other insurance will not pay. I realize I cannot appeal to
Medicare.
☐Option 3. NO I will not receive these items or services. I understand that you will not be able to submit a claim to
Medicare and that I will not be able to appeal your opinion that Medicare won’t pay.
Patient’s name
Identification Number
Signature of the patient or the authorized representative
Date
Form CMS 20014
OMB Exempt
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1