Written Medical Opinion For Employer Page 5
ADVERTISEMENT
Federal Register/Vol. 81, No. 58/Friday, March 25, 2016/Rules and Regulations
16883
and because they are caused by substantial
overexposures to respirable crystalline silica.
Although any case of silicosis indicates a
breakdown in prevention, a case of acute or
accelerated silicosis implies current high
exposure and a very marked breakdown in
prevention.
In addition to silicosis, employees exposed
to respirable crystalline silica, especially
those with accelerated or acute silicosis, are
at increased risks of contracting active TB
and other infections (ATS
1997;
Rees and
Murray
2007).
Exposure to respirable
crystalline silica also increases an employee's
risk of developing lung cancer, and the
higher the cumulative exposure, the higher
the risk (Steenland et al.
2001;
Steenland and
Ward
2014).
Symptoms for these diseases
and other respirable crystalline silica-related
diseases are discussed below.
1.2.
Chronic Silicosis. Chronic silicosis is
the most common presentation of silicosis
and usually occurs after at least
10
years of
exposure to respirable crystalline silica. The
clinical presentation of chronic silicosis is:
1.2.1.
Symptoms-shortness of breath and
cough, although employees may not notice
any symptoms early in the disease.
Constitutional symptoms, such as fever, loss
of appetite and fatigue, may indicate other
diseases associated with silica exposure,
such as TB infection or lung cancer.
Employees with these symptoms should
immediately receive further evaluation and
treatment.
1.2.2.
Physical Examination-may be
normal or disclose dry rales or rhonchi on
lung auscultation.
1.2.3.
Spirometry-may be normal or may
show only a mild restrictive or obstructive
pattern.
1.2.4.
Chest X-ray-classic findings are
small, rounded opacities in the upper lung
fields bilaterally. However, small irregular
opacities and opacities in other lung areas
can also occur. Rarely, "eggshell
calcifications" in the hilar and mediastinal
lymph nodes are seen.
1.2.5.
Clinical Course-chronic silicosis in
most cases is a slowly progressive disease.
Under the respirable crystalline silica
standard, the PLHCP is to recommend that
employees with a
1/0
category X-ray be
referred to an American Board Certified
Specialist in Pulmonary Disease or
Occupational Medicine. The PLHCP and/or
Specialist should counsel employees
regarding work practices and personal habits
that could affect employees' respiratory
health.
1.3.
Accelerated Silicosis. Accelerated
silicosis generally occurs within
5-10
years
of exposure and results from high levels of
exposure to respirable crystalline silica. The
clinical presentation of accelerated silicosis
is:
1.3.1.
Symptoms-shortness of breath,
cough, and sometimes sputum production.
Employees with exposure to respirable
crystalline silica, and especially those with
accelerated silicosis, are at high risk for
activation of TB infections, atypical
mycobacterial infections, and fungal
superinfections. Constitutional symptoms,
such as fever, weight loss, hemoptysis
(coughing up blood), and fatigue may herald
one of these infections or the onset of lung
cancer.
1.3.2.
Physical Examination-rales,
rhonchi, or other abnormal lung findings in
relation to illnesses present. Clubbing of the
digits, signs of heart failure, and car
pulmonale may be present in severe lung
disease.
1.3.3.
Spirometry-restrictive or mixed
restrictive/obstructive pattern.
1.3.4.
Chest X-ray-small rounded and/or
irregular opacities bilaterally. Large opacities
and lung abscesses may indicate infections,
lung cancer, or progression to complicated
silicosis, also termed progressive massive
fibrosis.
1.3.5.
Clinical Course-accelerated silicosis
has a rapid, severe course. Under the
respirable crystalline silica standard, the
PLHCP can recommend referral to a Board
Certified Specialist in either Pulmonary
Disease or Occupational Medicine, as
deemed appropriate, and referral to a
Specialist is recommended whenever the
diagnosis of accelerated silicosis is being
considered.
1.4.
Acute Silicosis. Acute silicosis is a rare
disease caused by inhalation of extremely
high levels of respirable crystalline silica
particles. The pathology is similar to alveolar
proteinosis with lipoproteinaceous material
accumulating in the alveoli. Acute silicosis
develops rapidly, often, within a few months
to less than
2
years of exposure, and is almost
always fatal. The clinical presentation of
acute silicosis is as follows:
1.4.1.
Symptoms-sudden, progressive,
and severe shortness of breath. Constitutional
symptoms are frequently present and include
fever, weight loss, fatigue, productive cough,
hemoptysis (coughing up blood), and
pleuritic chest pain.
1.4.2.
Physical Examination-dyspnea at
rest, cyanosis, decreased breath sounds,
inspiratory rales, clubbing of the digits, and
fever.
1.4.3.
Spirometry-restrictive or mixed
restrictive/obstructive pattern.
1.4.4.
Chest X-ray-diffuse haziness of the
lungs bilaterally early in the disease. As the
disease progresses, the "ground glass"
appearance of interstitial fibrosis will appear.
1.4.5.
Clinical Course-employees with
acute silicosis are at especially high risk of
TB activation, nontuberculous mycobacterial
infections, and fungal superinfections. Acute
silicosis is immediately life-threatening. The
employee should be urgently referred to a
Board Certified Specialist in Pulmonary
Disease or Occupational Medicine for
evaluation and treatment. Although any case
of silicosis indicates a breakdown in
prevention, a case of acute or accelerated
silicosis implies a profoundly high level of
silica exposure and may mean that other
employees are currently exposed to
dangerous levels of silica.
1.5.
COPD. COPD, including chronic
bronchitis and emphysema, has been
documented in silica-exposed employees,
including those who do not develop silicosis.
Periodic spirometry tests are performed to
evaluate each employee for progressive
changes consistent with the development of
COPD. In addition to evaluating spirometry
results of individual employees over time,
PLHCPs may want to be aware of general
trends in spirometry results for groups of
employees from the same workplace to
identify possible problems that might exist at
that workplace. (See Section 2 of this
Appendix on Medical Surveillance for
further discussion.) Heart disease may
develop secondary to lung diseases such as
COPD. A recent study by Liu et al.
2014
noted a significant exposure-response trend
between cumulative silica exposure and
heart disease deaths, primarily due to
pulmonary heart disease, such as car
pulmonale.
1.6. Renal and Immune System. Silica
exposure has been associated with several
types of kidney disease, including
glomerulonephritis, nephrotic syndrome, and
end stage renal disease requiring dialysis.
Silica exposure has also been associated with
other autoimmune conditions, including
progressive systemic sclerosis, systemic
lupus erythematosus, and rheumatoid
arthritis. Studies note an association between
employees with silicosis and serologic
markers for autoimmune diseases, including
antinuclear antibodies, rheumatoid factor,
and immune complexes Ualloul and Banks
2007;
Shtraichman et al.
2015).
1.7. TB
and Other Infections. Silica-
exposed employees with latent TB are
3
to
30
times more likely to develop active
pulmonary TB infection (ATS
1997;
Rees and
Murray
2007).
Although respirable
crystalline silica exposure does not cause TB
infection, individuals with latent TB
infection are at increased risk for activation
of disease if they have higher levels of
respirable crystalline silica exposure, greater
profusion of radiographic abnormalities, or a
diagnosis of silicosis. Demographic
characteristics, such as immigration from
some countries, are associated with increased
rates of latent TB infection. PLHCPs can
review the latest Centers for Disease Control
and Prevention (CDC) information on TB
incidence rates and high risk populations
online (See Section
5
of this Appendix).
Additionally, silica-exposed employees are at
increased risk for contracting nontuberculous
mycobacterial infections, including
Mycobacterium avium-intracellulare and
Mycobacterium kansaii.
1.8.
Lung Cancer. The National Toxicology
Program has listed respirable crystalline
silica as a known human carcinogen since
2000
(NTP
2014).
The International Agency
for Research on Cancer
(2012)
has also
classified silica as Group
1
(carcinogenic to
humans). Several studies have indicated that
the risk of lung cancer from exposure to
respirable crystalline silica and smoking is
greater than additive (Brown
2009;
Liu et al.
2013).
Employees should be counseled on
smoking cessation.
2. Medical Surveillance
PLHCPs who manage silica medical
surveillance programs should have a
thorough understanding of the many silica-
related diseases and health effects outlined in
Section
1
of this Appendix. At each clinical
encounter, the PLHCP should consider silica-
related health outcomes, with particular
vigilance for acute and accelerated silicosis.
In this Section, the required components of
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1 2
2 3
3 4
4 5
5 6
6 7
7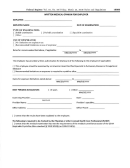 8
8








