Molina Healthcare Of Illinois Prior Authorization Request
ADVERTISEMENT
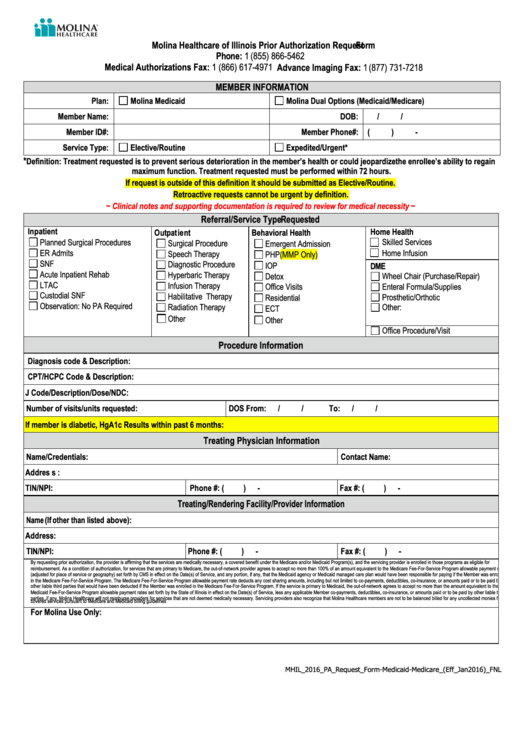
Molina Healthcare of Illinois Prior Authorization Request Form
Phone: 1 (855) 866-5462
Medical Authorizations Fax: 1 (866) 617-4971 Advance Imaging Fax: 1 (877) 731-7218
MEMBER INFORMATION
Plan:
Molina Medicaid
Molina Dual Options (Medicaid/Medicare)
Member Name:
DOB:
/
/
Member ID#:
Member Phone#:
(
)
-
Service Type:
Elective/Routine
Expedited/Urgent*
*
Definition: Treatment requested is to prevent serious deterioration in the member’s health or could jeopardize the enrollee’s ability to regain
maximum function. Treatment requested must be performed within 72 hours.
If request is outside of this definition it should be submitted as Elective/Routine.
Retroactive requests cannot be urgent by definition.
~ Clinical notes and supporting documentation is required to review for medical necessity ~
Referral/Service Type Requested
Inpatient
Home Health
Outpatient
Behavioral Health
Planned Surgical Procedures
Skilled Services
Surgical Procedure
Emergent Admission
ER Admits
Home Infusion
Speech Therapy
PHP(MMP Only)
SNF
Diagnostic Procedure
IOP
DME
Acute Inpatient Rehab
Hyperbaric Therapy
Detox
Wheel Chair (Purchase/Repair)
LTAC
Infusion Therapy
Office Visits
Enteral Formula/Supplies
Custodial SNF
Habilitative Therapy
Prosthetic/Orthotic
Residential
Observation: No PA Required
Radiation Therapy
Other:
ECT
Other
Other
Office Procedure/Visit
Procedure Information
Diagnosis code & Description:
CPT/HCPC Code & Description:
J Code/Description/Dose/NDC:
Number of visits/units requested:
DOS From:
/
/
To:
/
/
If member is diabetic, HgA1c Results within past 6 months:
Treating Physician Information
Name/Credentials:
Contact Name:
Address:
TIN/NPI:
Phone #: (
)
-
Fax #: (
)
-
Treating/Rendering Facility/Provider Information
Name (If other than listed above):
Address:
TIN/NPI:
Phone #: (
)
-
Fax #: (
)
-
By requesting prior authorization, the provider is affirming that the services are medically necessary, a covered benefit under the Medicare and/or Medicaid Program(s), and the servicing provider is enrolled in those programs as eligible for
reimbursement. As a condition of authorization, for services that are primary to Medicare, the out-of-network provider agrees to accept no more than 100% of an amount equivalent to the Medicare Fee-For-Service Program allowable payment rates
(adjusted for place of service or geography) set forth by CMS in effect on the Date(s) of Service, and any portion, if any, that the Medicaid agency or Medicaid managed care plan would have been responsible for paying if the Member was enrolled
in the Medicare Fee-For-Service Program. The Medicare Fee-For-Service Program allowable payment rate deducts any cost sharing amounts, including but not limited to co-payments, deductibles, co-insurance, or amounts paid or to be paid by
other liable third parties that would have been deducted if the Member was enrolled in the Medicare Fee-For-Service Program. If the service is primary to Medicaid, the out-of-network agrees to accept no more than the amount equivalent to the
Medicaid Fee-For-Service Program allowable payment rates set forth by the State of Illinois in effect on the Date(s) of Service, less any applicable Member co-payments, deductibles, co-insurance, or amounts paid or to be paid by other liable third
parties, if any. Molina Healthcare will not reimburse providers for services that are not deemed medically necessary. Servicing providers also recognize that Molina Healthcare members are not to be balanced billed for any uncollected monies for
covered services pursuant to Medicare and Medicaid billing guidelines
For Molina Use Only:
MHIL_2016_PA_Request_Form-Medicaid-Medicare_(Eff_Jan2016)_FNL
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1








