Department Of Insurance Prior Authorization Form In
ADVERTISEMENT
Indiana Register
DEPARTMENT OF INSURANCE
February 25, 2015
Bulletin 214
Prior Authorization
This bulletin is directed to all insurers writing policies of accident and sickness insurance, as defined by
IC
27-8-5-1; all health maintenance organizations (HMOs), as defined by
IC 27-13-1-19
and
IC
27-13-36.2-2(a); all
third-party administrators, including those defined at
IC
27-1-25-1(a) and those administering self-insured plans;
and other persons involved in reviewing claims and providing prior authorization for procedures. For purposes of
this bulletin, "prior authorization" will include any preapproval, preauthorization, prior approval, prior notification, or
similar requirement in a policy or contract; however, it does not include pretreatment payment estimates. The
purpose of this bulletin is to encourage all entities involved in the prior authorization process to use a common
form for prior authorization, thereby reducing costs to insurers and health care providers and avoiding
unnecessary delays for patients.
Prior authorization requests and subsequent approvals should be made in writing, which may include online
processes, electronic correspondence, facsimile correspondence, or other reproducible format, to avoid disputes
over oral representations. When a written request is not possible, prior authorization requests may be made by
phone or otherwise orally if the insurer allows. The Department has worked with representatives of insurers,
health care providers, and patients and has determined that the attached form, substantially similar to one already
in use in Texas, is a reasonable form for obtaining necessary information to make a determination on a prior
authorization request, whatever process is used. Therefore, the Department encourages insurers, HMOs,
administrators, and others to use the attached form.
Furthermore, the Department understands that no prior authorization is required by insurers for a patient with
a life-threatening condition; therefore, this form has no application in a life-threatening situation. If, during a prior
authorized surgical or other invasive procedure, a provider performs an additional related covered procedure due
to unforeseen medical necessity, the Department encourages insurers, HMOs, and TPAs not to deny coverage
solely for lack of prior approval, although the additional procedure was not included in the original prior approval.
Denials or partial denials should be explained to the requesting provider.
The Department is considering the adoption of an administrative rule that would require the use of a standard
prior authorization form for entities subject to the Department's jurisdiction. Voluntary use of the form following this
bulletin will provide practical experience and more valuable feedback during any rulemaking. Therefore, insurers
and others are urged to begin use of this form as soon as practicable.
Indiana Department of Insurance
______________________________________
Stephen W. Robertson, Commissioner
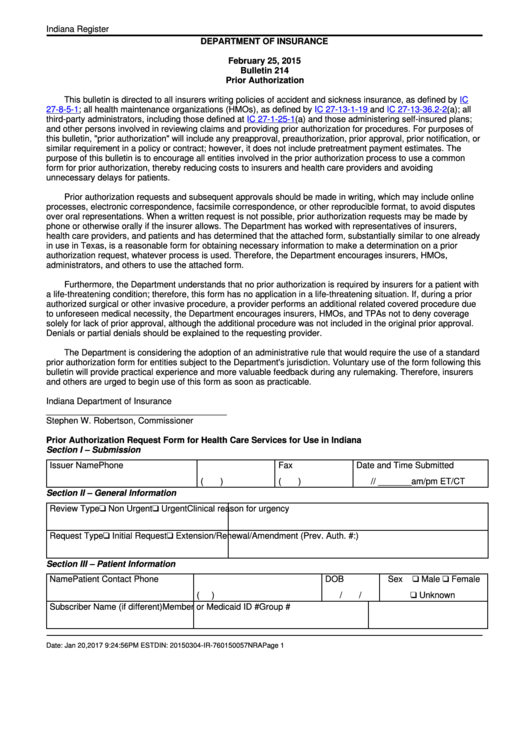
Prior Authorization Request Form for Health Care Services for Use in Indiana
Section I – Submission
Issuer Name
Phone
Fax
Date and Time Submitted
(
)
(
)
/
/ _______am/pm ET/CT
Section II – General Information
Review Type
Non Urgent
Urgent
Clinical reason for urgency
Request Type
Initial Request
Extension/Renewal/Amendment (Prev. Auth. #:
)
Section III – Patient Information
Name
Patient Contact Phone
DOB
Sex
Male
Female
(
)
/
/
Unknown
Subscriber Name (if different)
Member or Medicaid ID #
Group #
Date: Jan 20,2017 9:24:56PM EST
DIN: 20150304-IR-760150057NRA
Page 1
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1 2
2 3
3








