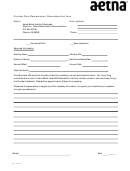
Virginia Provider Claim Reconsideration Form Page 2
ADVERTISEMENT
Aetna Better Health® of Virginia
9881 Mayland Drive
Richmond, VA 23233
Claim/Reconsideration Descriptions
Itemized Bill
All claims associated with an Itemized Bill must be broken out per Rev code to verify charges billed on the
UB match the charges billed on the Itemized bill. (Please attach I-Bill that is broken out by rev code with
sub-totals.)
Duplicate Claim
Review request for a claim whose original reason for denial was “duplicate.”
Provide documentation as to why the claim or service is not a duplicate such as medical records showing
two services were performed.
Corrected Claim
The corrected claim must be clearly identified as a corrected claim by writing or stamping “corrected” on
the claim itself.
Coordination of Benefits
Attach EOB or letter from primary carrier and forward to the claims department identifying as “corrected”
claim.
Proof of Timely Filing
For electronically submitted claims provide the second level acceptance report.
Refer to Proof of Timely Filing Requirements in your Provider Manual.
Claim/Coding Edit
Aetna Better Health of Virginia uses two (2) claims edit applications: Claim Check and iHealth. Please
refer to the Provider Manual on the Aetna Better Health of Virginia website
for more information on claim editing.
Corrected claims must be received within 365 of the date on the first remittance advice. Please refer to
the Aetna Better Health of Virginia Provider Manual at , Claims
and Reimbursement Procedures section for more information.
Appeals must be received within 30 days of the date of the incident causing the appeal. Please refer to
the Aetna Better Health of Virginia Provider Manual online at .
VA-16-04-02
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Business
 1
1 2
2