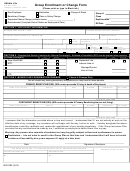
Form Gef040 - Group Enrollment Page 2
ADVERTISEMENT
Instructions for completing the Group Enrollment Form
DESIRED ACTION - Check the appropriate action and indicate the Date(s) in the space provided. An Event Date is the date of a specific occurrence, due to
change in status, marriage, divorce, birth or adoption, group's anniversary date, or rate change. Your request must be received within 30 days of the Event
Date. Please see your Group Representative for events that fall outside the 30-day period. If New Add Subscriber, Add Dependent or Change Coverage,
you must also check Desired Coverage and Persons covered, and Family Member Information section.
Cancel Request
To process a Subscriber or Member Cancellation, please use the Membership Cancellation Worksheet - OR -
To Cancel an Employee/Subscriber using the
To Cancel a Dependent using the
Group Enrollment Form:
Group Enrollment Form:
Check Cancel Subscriber (S) Box
Check Cancel Dependent (M) box
Check Products to be cancelled (Medical, Dental)
Check Products to be cancelled (Medical, Dental)
Indicate Reason Code in space provided (See codes below)
Indicate Reason Code in space provided (see codes below)
Indicate Cancellation Date in space provided
Indicate Cancellation Date in space provided
Complete Subscriber Information
Complete Subscriber Information
Complete Member Name and Member Birthdate
Cancel Subscriber Reasons
Cancel Dependent Reasons
CE – Cobra End Date (29)
CB – COBRA Begin Date
LE – Left Employer/No Longer(11)
MA – Marriage (25)
CP – Commercial (09)
MR – Subscriber Request (02)
SD – Subscriber Deceased (05)
OA – Dependent Over Age (20)
SB – Spouse's Excellus BCBS
DV – Divorce (25)
SR – Subscriber Request (02)
DM – Deceased (05)
MC – Medicaid
MX – Medicare (03)
CB – Cobra Begin Date
MS – Ineligible Student (28)
MX – Medicare (03)
CD – Cobra Disabled Date
If the only change is one of the following, please call Customer Service at the telephone number indicated on your identification card. A Group Enrollment Form is not required.
Address
Birthdate
PCP or OB/GYN
DESIRED COVERAGE
All products may not be applicable to your employer group. Please check with your Group Representative.
SUBSCRIBER
If you or your dependents are Medicare eligible, complete the Medicare Eligible-Group Enrollment Form. If you are disabled, see your
Group Representative to determine eligibility for OBRA. If eligible, complete the appropriate form.
FAMILY MEMBER QUALIFIED GUIDELINES:
If there are more than three members please use an additional form.
A legal spouse (an ex-spouse is not a qualified member as of the divorce date)
Must be under the dependent and student age for your employer group
- Unmarried child, natural, adopted or stepchild
- A full-time student (indicate under Relationship)
- Chiefly dependent upon you for support
Other: The following dependents have additional eligibility requirements.
Dependents pending adoption, grandchild dependent*, dependents for whom employee/subscriber has legal custody or legal guardianship, or a
dependent who is claimed on subscriber’s current federal income tax return, or a disabled dependent who is over the dependent age for your employer
group. Please contact Customer Service for the appropriate form.
*if supporting documentation is attached.
RELEASE
I am applying to enroll myself and my eligible dependents, if any, under the medical and/or dental contract.
In the event that a premium contribution is required of me, I agree to pay the premium amounts applicable to the contract
under which I am covered. I authorize my employer to deduct from my payroll such applicable amounts and to remit them
to Excellus BlueCross BlueShield.
If this application is made on behalf of a minor, the responsible party must complete the application.
By accepting this contract, I grant permission to Excellus BlueCross BlueShield to submit charges to and/or recover
payment from any other insurance carrier acting as my primary insurer.
I authorize Excellus BlueCross BlueShield to request and receive medical or dental information regarding me or my
covered dependents from my healthcare practitioner or healthcare institution either orally or in writing and to use this
information for providing coverage. Providing coverage includes: processing claims, reviewing grievances or complaints
involving care and quality assurance reviews of care, whether based on a specific complaint or a routine audit of randomly
selected cases. In the use of data for these purposes, we may transmit personal information to third parties with which we
contract, including pharmacy benefit managers, disease management vendors or surveyors.
I hereby represent that all information furnished by me hereon is true and complete to the best of my knowledge.
The certificate or contract for which application is being made may impose a waiting period of up to twelve (12) months for
preexisting conditions, subject to the provisions of applicable law including creditable coverage requirements. The
certificate or contract document will describe any applicable waiting periods.
EMPLOYER INFORMATION
This section to be completed by the Employer Group Representative.
Complete only the coverage section (Medical, Dental) that is applicable to the employee's request.
If you have any questions, please contact Customer Service
Traditional or Comprehensive: 1-800-765-5226
HMO or Point of Service: 1-800-722-7884
PPO: 1-877-381-8659
Membership Inquiries:
1-800-765-5224
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Business
 1
1 2
2