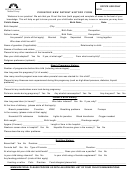
New Patient History Form Page 2
ADVERTISEMENT
Review of Systems: Circle all the symptoms listed below that you are CURRENTLY having.
General:
chills, fatigue, fever, night sweats, weight gain, weight loss
Allergy/Immunology:
immune deficiency, environmental allergies
Eyes:
blurry vision, eye pain
runny nose, congestion, difficulty swallowing, ear pain, ringing in ears,
Ears, Nose, Mouth:
sore throat
increased hunger, hair loss, cold intolerance, excessive thirst,
Endocrine:
heat intolerance
Respiratory:
shortness of breath, cough, wheezing, snoring
Breast:
breast lump, breast pain, nipple discharge, breast skin changes
Cardiovascular:
leg pain with walking, chest pain, fluid accumulation, palpitations
hernia, abdominal pain, blood in stools, constipation, diarrhea,
Gastrointestinal:
heartburn, nausea, vomiting
Hematology/Oncology:
frequent infections, easy bruising, easy bleeding
pelvic pain, menopause symptom, abnormal periods, genital sores,
Reproductive - Female:
vaginal discharge
Reproductive - Male:
erectile dysfunction, testicular pain, penile discharge, genital sores
Urinary:
blood in urine, difficulty urinating, kidney stones, bladder/kidney infections
Musculoskeletal:
recent trauma, muscle aches, joint pain, joint swelling
Skin:
discoloration, itching, rash, change in moles or spots
difficulty speaking, fainting, headache, loss of strength, memory loss,
Neurological:
tingling/numbness, tremor/shake
Psychological:
anxiety, depression, difficulty sleeping, physical or mental abuse
Other Problems
Brief description:
No Symptoms
I am having no problems today
Family History (list all health problems known, if deceased list age at death):
**Please list any known family medical problems below.**
Mother: _____________________________________
Father: _____________________________________
Siblings: __________________________________________________________________________________
Children: _________________________________________________________________________________
Grandparents: ________________________________
Aunt/Uncle: _________________________________
Other: ____________________________________________________________________________________
__ Check if adopted and family history unknown
Social History:
__ Smoker (packs per day): _______
__ Alcohol (drinks per week): _______
__ Street Drugs: __________
__ Snuff/chew (cans per day): _____
__ eCigarette/Vapor
Patient/Guardian Signature: ___________________________________ Date: ______________________
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1 2
2 3
3 4
4