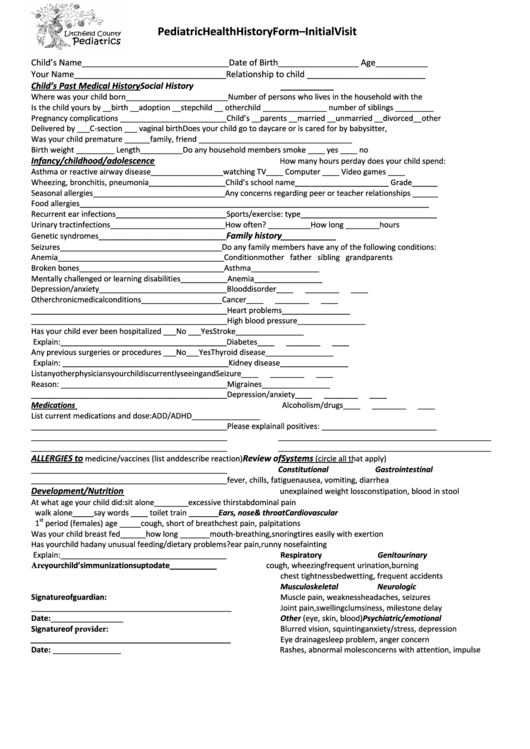
Pediatric Health History Form - Initial Visit
ADVERTISEMENT
Pediatric Health History Form – Initial Visit
Child’s Name_______________________________
Date of Birth_________________ Age___________
Your Name________________________________
Relationship to child _________________________
Child’s Past Medical History
Social History
Where was your child born________________________
Number of persons who lives in the household with the
Is the child yours by __birth __adoption __stepchild __ other
child _______________ number of siblings _________
Pregnancy complications _________________________
Child’s __parents __married __unmarried __divorced __other
Delivered by ___C-section ___ vaginal birth
Does your child go to daycare or is cared for by babysitter,
Was your child premature ______
family, friend ____________________________________
Birth weight _________ Length __________
Do any household members smoke ____ yes ____ no
Infancy/childhood/adolescence
How many hours per day does your child spend:
Asthma or reactive airway disease_________________
watching TV____ Computer ____ Video games ____
Wheezing, bronchitis, pneumonia__________________
Child’s school name______________________ Grade______
Seasonal allergies_______________________________
Any concerns regarding peer or teacher relationships ______
Food allergies__________________________________
________________________________________________
Recurrent ear infections__________________________
Sports/exercise: type________________________________
Urinary tract infections___________________________
How often? __________ How long ________hours
Family history
Genetic syndromes______________________________
Seizures______________________________________
Do any family members have any of the following conditions:
Anemia_______________________________________
Condition
mother father sibling grandparents
Broken bones__________________________________
Asthma
____
____ ____
____
Mentally challenged or learning disabilities___________
Anemia
____
____ ____
____
Depression/anxiety______________________________
Blood disorder
____
____
____
____
Other chronic medical conditions___________________
Cancer
____
____
____
____
______________________________________________
Heart problems
____
____
____
____
______________________________________________
High blood pressure ____
____
____
____
Has your child ever been hospitalized ___No ___Yes
Stroke
____
____ ____
____
Explain: _______________________________________
Diabetes
____
____
____
____
Any previous surgeries or procedures ___No ___Yes
Thyroid disease
____
____
____
____
Explain: _______________________________________
Kidney disease
____
____
____
____
List any other physicians your child is currently seeing and
Seizure
____
____ ____
____
Reason: _______________________________________
Migraines
____
____
____
____
______________________________________________
Depression/anxiety ____
____
____
____
Medications
Alcoholism/drugs
____
____
____
____
List current medications and dose:
ADD/ADHD
____
____
____
____
______________________________________________
Please explain all positives: ___________________________
______________________________________________
__________________________________________________
______________________________________________
__________________________________________________
ALLERGIES to
Review of Systems
medicine/vaccines (list and describe reaction)
(circle all that apply)
______________________________________________
Constitutional
Gastrointestinal
______________________________________________
fever, chills, fatigue
nausea, vomiting, diarrhea
Development/Nutrition
unexplained weight loss
constipation, blood in stool
At what age your child did: sit alone________
excessive thirst
abdominal pain
walk alone_____ say words ____ toilet train _______
Ears, nose & throat
Cardiovascular
st
1
period (females) age _____
cough, short of breath
chest pain, palpitations
Was your child breast fed______ how long _______
mouth-breathing, snoring tires easily with exertion
Has your child had any unusual feeding/dietary problems?
ear pain, runny nose
fainting
Explain: _______________________________________
Respiratory
Genitourinary
Are your child’s immunizations up to date ___________
cough, wheezing
frequent urination, burning
chest tightness
bedwetting, frequent accidents
Musculoskeletal
Neurologic
Signature of guardian:
Muscle pain, weakness
headaches, seizures
_______________________________________________
Joint pain, swelling
clumsiness, milestone delay
Date: _________________
Other (eye, skin, blood)
Psychiatric/emotional
Signature of provider:
Blurred vision, squinting
anxiety/stress, depression
_______________________________________________
Eye drainage
sleep problem, anger concern
Date: ________________
Rashes, abnormal moles
concerns with attention, impulse
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1








