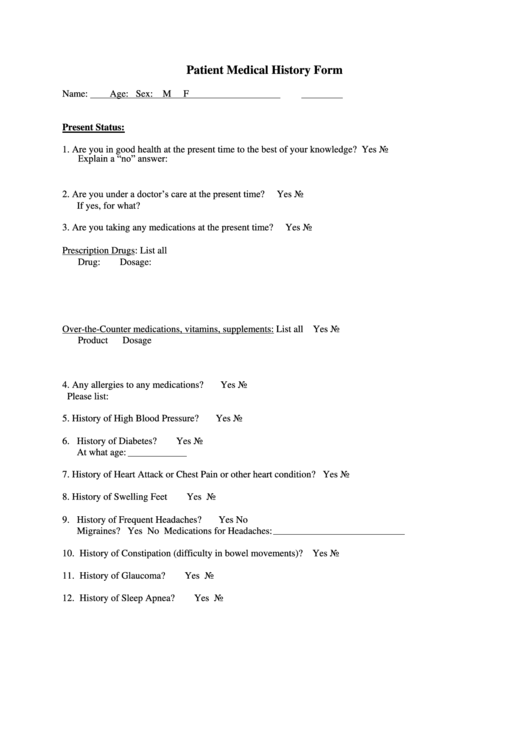
Patient Medical History Form
ADVERTISEMENT
Patient Medical History Form
Name:
Age:
Sex: M
F
Present Status:
1. Are you in good health at the present time to the best of your knowledge?
Yes
No
Explain a “no” answer:
2. Are you under a doctor’s care at the present time?
Yes
No
If yes, for what?
3. Are you taking any medications at the present time?
Yes
No
Prescription Drugs: List all
Drug:
Dosage:
Over-the-Counter medications, vitamins, supplements: List all
Yes
No
Product
Dosage
4. Any allergies to any medications?
Yes
No
Please list:
5. History of High Blood Pressure?
Yes
No
6. History of Diabetes?
Yes
No
At what age:
7. History of Heart Attack or Chest Pain or other heart condition?
Yes
No
8. History of Swelling Feet
Yes
No
9. History of Frequent Headaches?
Yes
No
Migraines? Yes No Medications for Headaches:
10. History of Constipation (difficulty in bowel movements)?
Yes
No
11. History of Glaucoma?
Yes
No
12. History of Sleep Apnea?
Yes
No
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1 2
2 3
3 4
4 5
5








