Bedside Shift Report Checklist
ADVERTISEMENT
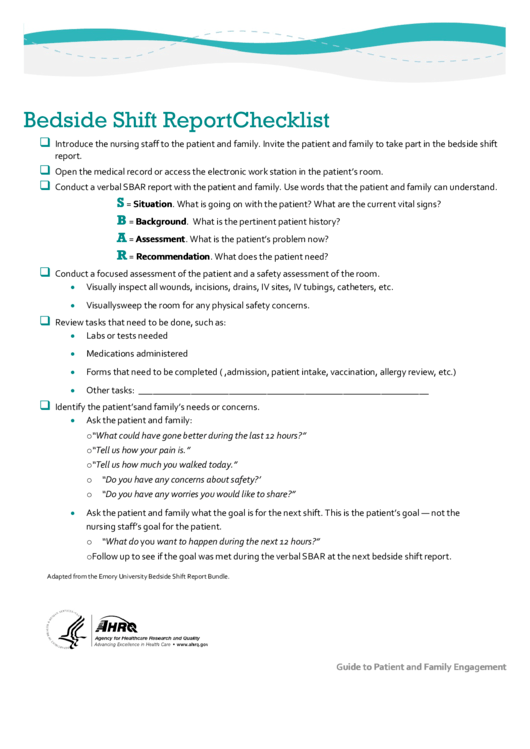
Bedside Shift Report Checklist
Introduce the nursing staff to the patient and family. Invite the patient and family to take part in the bedside shift
report.
Open the medical record or access the electronic work station in the patient’s room.
Conduct a verbal SBAR report with the patient and family. Use words that the patient and family can understand.
S
= Situation. What is going on with the patient? What are the current vital signs?
B
= Background. What is the pertinent patient history?
A
= Assessment. What is the patient’s problem now?
R
= Recommendation. What does the patient need?
Conduct a focused assessment of the patient and a safety assessment of the room.
•
Visually inspect all wounds, incisions, drains, IV sites, IV tubings, catheters, etc.
•
Visually sweep the room for any physical safety concerns.
Review tasks that need to be done, such as:
•
Labs or tests needed
•
Medications administered
•
Forms that need to be completed (e.g., admission, patient intake, vaccination, allergy review, etc.)
•
Other tasks: _____________________________________________________________
Identify the patient’s and family’s needs or concerns.
•
Ask the patient and family:
o “What could have gone better during the last 12 hours?”
o “Tell us how your pain is.”
o “Tell us how much you walked today.”
o “Do you have any concerns about safety?’
o “Do you have any worries you would like to share?”
•
Ask the patient and family what the goal is for the next shift. This is the patient’s goal — not the
nursing staff’s goal for the patient.
o “What do you want to happen during the next 12 hours?”
o Follow up to see if the goal was met during the verbal SBAR at the next bedside shift report.
Adapted from the Emory University Bedside Shift Report Bundle.
Guide to Patient and Family Engagement
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Life
 1
1