Nursing Admission Assessment Template
ADVERTISEMENT
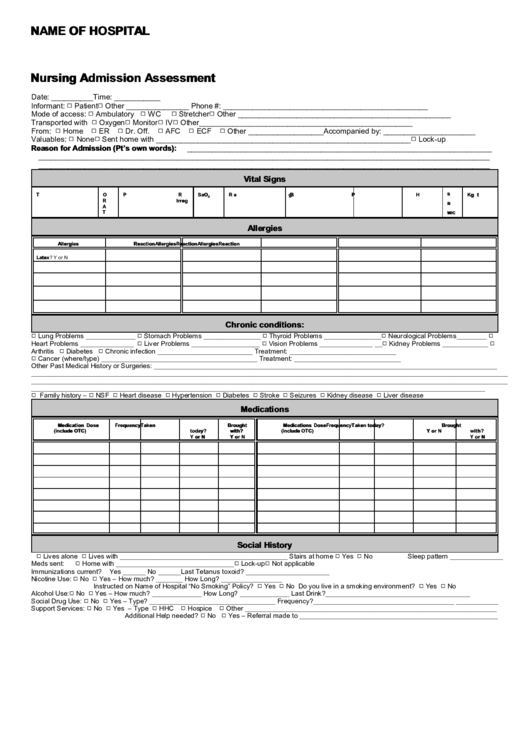
NAME OF HOSPITAL
Nursing Admission Assessment
Date: __________Time: ___________
'
'
Informant:
Patient
Other _______________ Phone #:
_________________________________________________
'
'
'
'
Mode of access:
Ambulatory
WC
Stretcher
Other
___________________________________________________
'
'
'
'
Transported with
Oxygen
Monitor
IV
Other ___________________________________________________
'
'
'
'
'
'
From:
Home
ER
Dr. Off.
AFC
ECF
Other __________________
Accompanied by: ______________________
'
'
'
Valuables:
None
Sent home with _____________________________________________________________
Lock-up
Reason for Admission (Pt’s own words):
_________________________________________________________________________
____________________________________________________________________________________________________________
____________________________________________________________________________________________________________
Vital Signs
T
O
P
Reg
SaO
R
BP
Ht
Wt
S
Kg
2
R
Irreg
B
A
T
W/C
Allergies
Allergies
Reaction
Allergies
Reaction
Allergies
Reaction
Latex? Y or N
Chronic conditions:
'
'
'
'
'
Lung Problems _____________
Stomach Problems _______________
Thyroid Problems _______________
Neurological Problems________
'
'
'
'
Heart Problems ______________
Liver Problems __________________
Vision Problems ______________ __
Kidney Problems ____________
'
'
Arthritis
Diabetes
Chronic infection _________________________ Treatment:
____________________________
'
Cancer (where/type) _________________________________________ Treatment:
____________________________
Other Past Medical History or Surgeries: __________________________________________________________________________________________
_____________________________________________________________________________________________________________________________
_____________________________________________________________________________________________________________________________
_______________________________________________________________________________________________________________________
'
'
'
'
'
'
'
'
'
Family history –
NSF
Heart disease
Hypertension
Diabetes
Stroke
Seizures
Kidney disease
Liver disease
Medications
Medication
Dose
Frequency
Taken
Brought
Medications
Dose
Frequency
Taken today?
Brought
(include OTC)
today?
with?
(include OTC)
Y or N
with?
Y or N
Y or N
Y or N
Social History
'
'
'
'
Lives alone
Lives with ____________________________________________ Stairs at home
Yes
No
Sleep pattern ______________
'
'
'
Meds sent:
Home with _______________________________
Lock-up
Not applicable
Immunizations current?
Yes ______ No ______
Last Tetanus toxoid? ______________________
'
'
Nicotine Use:
No
Yes – How much? _______ How Long? ________________
'
'
'
'
Instructed on Name of Hospital “No Smoking” Policy?
Yes
No Do you live in a smoking environment?
Yes
No
'
'
Alcohol Use:
No
Yes – How much? _____________ How Long? _____________ Last Drink?
______________________________________
'
'
Social Drug Use:
No
Yes – Type? _________________________________ Frequency?
_____________________________________ ___________
'
'
'
'
'
Support Services:
No
Yes – Type
HHC
Hospice
Other
__________________________________________________________________
'
'
Additional Help needed?
No
Yes – Referral made to
____________________________________________________
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1 2
2 3
3 4
4 5
5








