Out-Of-Network Claim Form Date Of Service - The Standard
ADVERTISEMENT
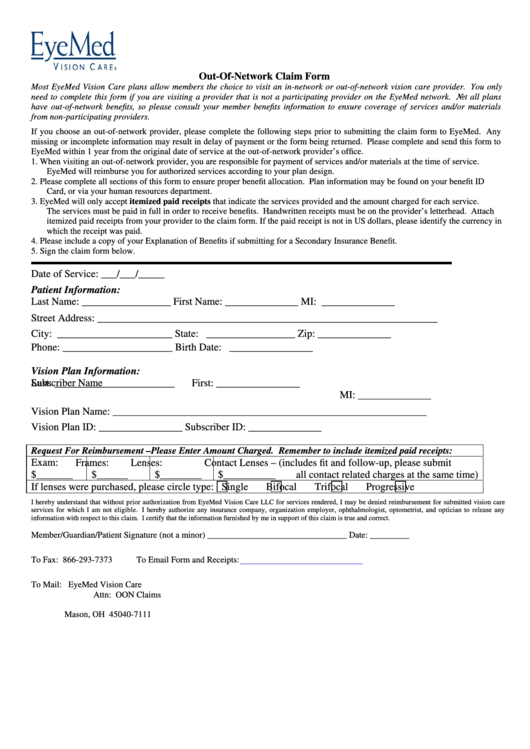
Out-Of-Network Claim Form
Most EyeMed Vision Care plans allow members the choice to visit an in-network or out-of-network vision care provider. You only
need to complete this form if you are visiting a provider that is not a participating provider on the EyeMed network. Not all plans
have out-of-network benefits, so please consult your member benefits information to ensure coverage of services and/or materials
from non-participating providers.
If you choose an out-of-network provider, please complete the following steps prior to submitting the claim form to EyeMed. Any
missing or incomplete information may result in delay of payment or the form being returned. Please complete and send this form to
EyeMed within 1 year from the original date of service at the out-of-network provider’s office.
1. When visiting an out-of-network provider, you are responsible for payment of services and/or materials at the time of service.
EyeMed will reimburse you for authorized services according to your plan design.
2. Please complete all sections of this form to ensure proper benefit allocation. Plan information may be found on your benefit ID
Card, or via your human resources department.
3. EyeMed will only accept itemized paid receipts that indicate the services provided and the amount charged for each service.
The services must be paid in full in order to receive benefits. Handwritten receipts must be on the provider’s letterhead. Attach
itemized paid receipts from your provider to the claim form. If the paid receipt is not in US dollars, please identify the currency in
which the receipt was paid.
4. Please include a copy of your Explanation of Benefits if submitting for a Secondary Insurance Benefit.
5. Sign the claim form below.
Date of Service: ___/___/_____
Patient Information:
Last Name: _________________
First Name: ______________
MI: ______________
Street Address: _________________________________________________________________
City: ______________________
State: _________________
Zip: ______________
Phone: _____________________
Birth Date: ________________
Vision Plan Information:
Subscriber Name
Last: _______________________
First: ________________
MI: ______________
Vision Plan Name: ____________________________________________________________
Vision Plan ID: ________________ Subscriber ID: ______________
Request For Reimbursement –Please Enter Amount Charged. Remember to include itemized paid receipts:
Exam:
Frames:
Lenses:
Contact Lenses – (includes fit and follow-up, please submit
$_______
$______
$________
$__________
all contact related charges at the same time)
If lenses were purchased, please circle type:
Single
Bifocal
Trifocal
Progressive
I hereby understand that without prior authorization from EyeMed Vision Care LLC for services rendered, I may be denied reimbursement for submitted vision care
services for which I am not eligible. I hereby authorize any insurance company, organization employer, ophthalmologist, optometrist, and optician to release any
information with respect to this claim. I certify that the information furnished by me in support of this claim is true and correct.
Member/Guardian/Patient Signature (not a minor) ________________________________ Date: _________
To Fax: 866-293-7373
To Email Form and Receipts:
To Mail:
EyeMed Vision Care
Attn: OON Claims
P.O. Box 8504
Mason, OH 45040-7111
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Legal
 1
1 2
2