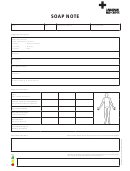
Patient Assessment & Soap Note Template
ADVERTISEMENT
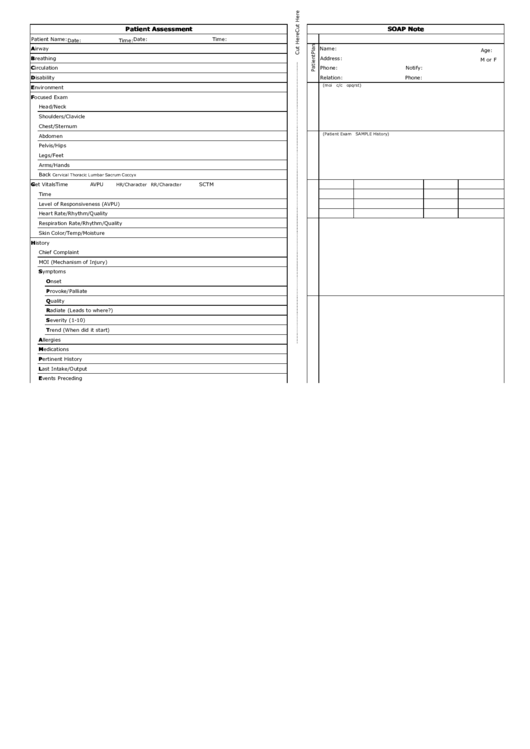
Patient Assessment
SOAP Note
Patient Name:
Date:
Time:
Date:
Time:
Airway
Name:
Age:
Breathing
Address:
M or F
Circulation
Phone:
Notify:
Disability
Relation:
Phone:
(moi c/c opqrst)
Environment
Focused Exam
Head/Neck
Shoulders/Clavicle
Chest/Sternum
(Patient Exam SAMPLE History)
Abdomen
Pelvis/Hips
Legs/Feet
Arms/Hands
Back
Cervical Thoracic Lumbar Sacrum Coccyx
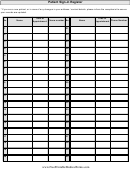
Get Vitals
Time
AVPU
SCTM
HR/Character RR/Character
Time
Level of Responsiveness (AVPU)
Heart Rate/Rhythm/Quality
Respiration Rate/Rhythm/Quality
Skin Color/Temp/Moisture
History
Chief Complaint
MOI (Mechanism of Injury)
Symptoms
Onset
Provoke/Palliate
Quality
Radiate (Leads to where?)
Severity (1-10)
Trend (When did it start)
Allergies
Medications
Pertinent History
Last Intake/Output
Events Preceding
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1 2
2