Soap Note Template
ADVERTISEMENT
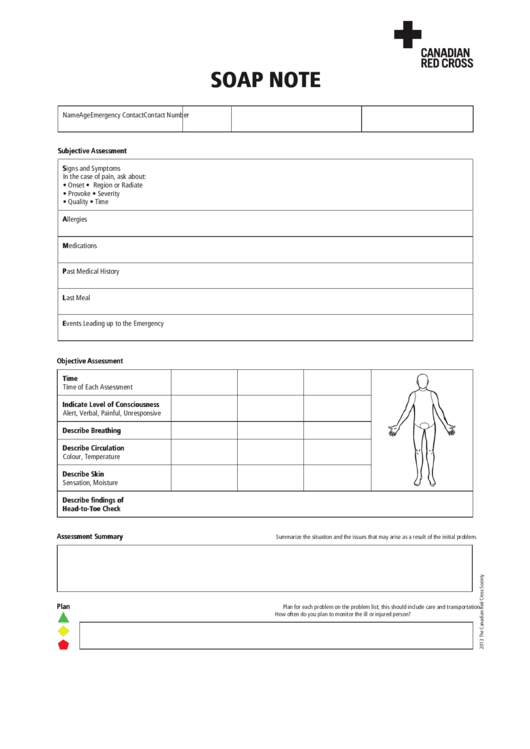
SOAP NOTE
Name
Age
Emergency Contact
Contact Number
Subjective Assessment
Signs and Symptoms
In the case of pain, ask about:
• Onset
• Region or Radiate
• Provoke
• Severity
• Quality
• Time
Allergies
Medications
Past Medical History
Last Meal
Events Leading up to the Emergency
Objective Assessment
Time
Time of Each Assessment
Indicate Level of Consciousness
Alert, Verbal, Painful, Unresponsive
Describe Breathing
Describe Circulation
Colour, Temperature
Describe Skin
Sensation, Moisture
Describe findings of
Head-to-Toe Check
Assessment Summary
Summarize the situation and the issues that may arise as a result of the initial problem.
Plan
Plan for each problem on the problem list; this should include care and transportation.
How often do you plan to monitor the ill or injured person?
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1








