Your Out-Of-Canada Claim
ADVERTISEMENT
Your Out-of-Canada Claim
All Out-of-Canada (OOC) & Out-of-Province claims must be submitted directly to your "Travel Assist" OOC service
provider, Allianz Global Assistance, using their claim form.
Please follow these steps:
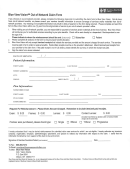
1. Fully complete the attached Allianz Global Assistance Emergency Medical Expense claim, indicating your
RWAM group/certificate number on the form.
2. Since your OOC benefit includes a maximum number of days per trip that you are covered for from the day you
leave your province of residence, proof of this departure date will be requested by Allianz Global Assistance if
your claim exceeds $1000. To expedite any such claim, 'proof of departure' documents should accompany
your claim form. Such proof may include:
• dated airline, train or bus ticket receipts
• if you travelled via automobile, dated receipts for gas or meals purchased by you
• any other dated receipts confirming your last date in your Canadian home province prior to your departure
3. As proof of coverage under your provincial health care plan, attach to the claim a photocopy of the applicable
claimant’s Provincial Health Card.
4. It is recommended that you photocopy your completed Allianz Global Assistance claim form and all documents
before submitting your claim, and keep the copies for your own records and reference.
5. Attach your original (i.e. not copies) itemized medical bills and prescription receipts to the completed claim form
and mail to:
Allianz Global Assistance
P.O. Box 277
Waterloo, ON
N2J 4A4
Please Note:
OOC claims generally take longer to process than typical processing times you may be accustomed to for other
claims such as EHC or Dental. Allianz Global Assistance may require further information from you, or directly
from the invoicing treatment provider. Depending upon the provider and/or the country in which treatment took
place, it may take a significant period of time for Allianz Global Assistance to obtain the required information.
However their procedures include follow-ups every 21 days from the date information was originally requested,
until they receive the required documentation. At that point, their claim turnaround time is 10 business days from
date of receipt of all required documentation.
Should you receive any notices, invoices or related correspondence directly from your OOC invoicing treatment
provider, please contact RWAM. On your behalf, we will ask Allianz Global Assistance to address the provider’s
inquiry directly.
Call: RWAM INSURANCE ADMINISTRATORS INC.
Attention: Heather Aguiar @ Ext #221
Local:
519-669-1632
Toll-free: 1-877-888-RWAM (7926)
RWAM 02.12
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Business
 1
1 2
2 3
3