Member Claim Form - Cigna Healthcare Page 2
ADVERTISEMENT
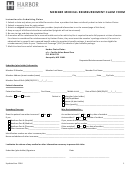
INSTRUCTIONS FOR FILING A CLAIM
IMPORTANT
1.
This form can be used for all medical plans. This form only needs to be completed if the provider is not submitting the
claim on your behalf. Out-of-network claims can be submitted by the provider if the provider is able and willing to file on
your behalf.
2. If you received this claim form electronically, you can fill in the fields by clicking to the right of the first field (Employee’s
Name) and typing in the information. Remember to click on the Clear Fields button on the top of page 1 after printing out
the completed claim form.
3.
If you are completing this form by hand, use a new printed form rather than a photocopy to ensure the form can be
scanned into our system. Also, be sure to print clearly and use black ink when you complete the form.
Claim must be postmarked within one year of your date of service for claims to be considered payable.
4.
5.
Use a separate claim form for each provider and each member of the family. A new form can be obtained from
under HealthCare, Important Forms or by calling Member Services using the toll-free number on your
CIGNA ID card.
6.
Your claim cannot be processed without your ID Number (Employee Section, Block D). Please reference the front of your
CIGNA ID card to find this number. Your ID may be the employee’s Social Security Number.
7.
You must submit an itemized bill for your claim to be processed. Receipts, balance due statements and cancelled checks
are not acceptable replacements for the itemized bill.
8.
ITEMIZED BILLS MUST INCLUDE:
Employee Name
Date of Service
Provider Name
Patient Name
Provider Address
Diagnosis
Type of Service
Provider Tax ID Number
Charge for Service
9. We suggest you make a copy of your bill(s) and your completed claim form for your records. If you are submitting one
claim, please do not paper clip or staple your claim form and bill(s). If you are submitting multiple claims in one envelope,
please paper clip the appropriate claim form and itemized bill(s) together.
10.
Please be aware that payment will be sent to the provider, unless the provider is non-contracted with CIGNA and you
submit a receipt that shows you paid in full (a zero balance) with your itemized bill and this claim form. CIGNA reserves
the right to request additional documentation, such as medical records prior to processing your claim.
11. If the patient has coverage through another health insurance carrier which is considered primary (CIGNA as secondary),
you must submit the Explanation of Benefits (EOB) from the insurance carrier for this service along with this completed
form and itemized bill.
EXPLANATION OF BENEFITS
You will receive an Explanation of Benefits (EOB) after your claim is processed explaining the charges applied to your
deductible and any charges you owe to the provider. Please keep your EOBs for later reference.
MAILING INSTRUCTIONS
If you are submitting one claim, please do not paper clip or staple your claim form and bill(s). If you are submitting multiple
claims in one envelope, please paper clip the appropriate claim form and itemized bill(s) together.
Send your completed claim form and itemized bill(s) to the CIGNA address listed on your identification card.
If you have additional questions, please contact Member Services using the toll-free number on your ID card.
591692a Rev. 10/2008
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Legal
 1
1 2
2 3
3