Insurance Verification For Physical Therapy Benefits
ADVERTISEMENT
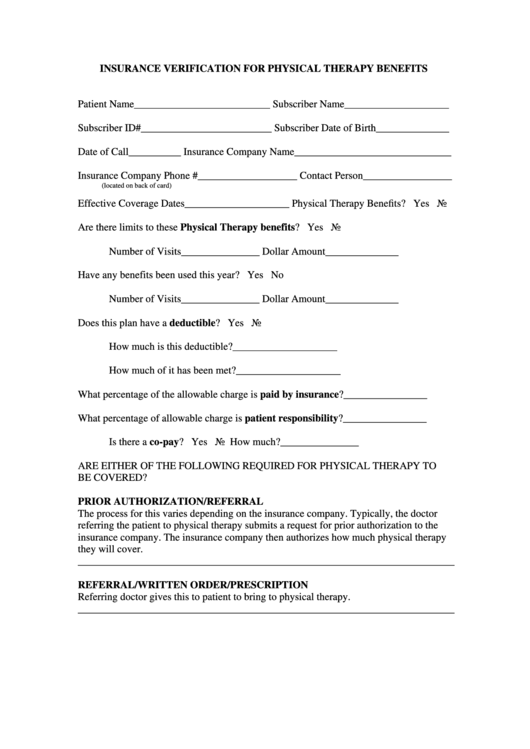
INSURANCE VERIFICATION FOR PHYSICAL THERAPY BENEFITS
Patient Name__________________________ Subscriber Name____________________
Subscriber ID#_________________________ Subscriber Date of Birth______________
Date of Call__________ Insurance Company Name______________________________
Insurance Company Phone #___________________ Contact Person_________________
(located on back of card)
Effective Coverage Dates____________________ Physical Therapy Benefits? Yes No
Are there limits to these Physical Therapy benefits? Yes No
Number of Visits_______________ Dollar Amount______________
Have any benefits been used this year? Yes No
Number of Visits_______________ Dollar Amount______________
Does this plan have a deductible? Yes No
How much is this deductible?____________________
How much of it has been met?____________________
What percentage of the allowable charge is paid by insurance?________________
What percentage of allowable charge is patient responsibility?________________
Is there a co-pay? Yes No
How much?_______________
ARE EITHER OF THE FOLLOWING REQUIRED FOR PHYSICAL THERAPY TO
BE COVERED?
PRIOR AUTHORIZATION/REFERRAL
The process for this varies depending on the insurance company. Typically, the doctor
referring the patient to physical therapy submits a request for prior authorization to the
insurance company. The insurance company then authorizes how much physical therapy
they will cover.
________________________________________________________________________
REFERRAL/WRITTEN ORDER/PRESCRIPTION
Referring doctor gives this to patient to bring to physical therapy.
________________________________________________________________________
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Legal
 1
1








