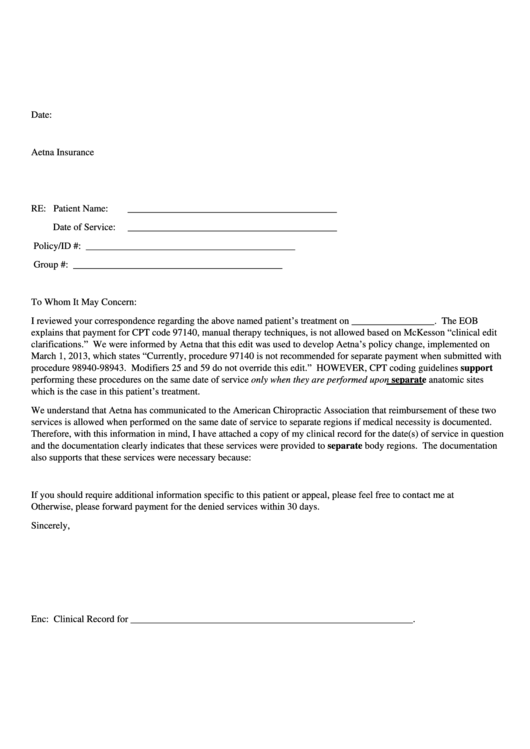
Date:
Aetna Insurance
RE:
Patient Name:
___________________________________________
Date of Service:
___________________________________________
Policy/ID #:
___________________________________________
Group #:
___________________________________________
To Whom It May Concern:
I reviewed your correspondence regarding the above named patient’s treatment on _________________. The EOB
explains that payment for CPT code 97140, manual therapy techniques, is not allowed based on McKesson “clinical edit
clarifications.” We were informed by Aetna that this edit was used to develop Aetna’s policy change, implemented on
March 1, 2013, which states “Currently, procedure 97140 is not recommended for separate payment when submitted with
procedure 98940-98943. Modifiers 25 and 59 do not override this edit.” HOWEVER, CPT coding guidelines support
performing these procedures on the same date of service only when they are performed upon separate anatomic sites
which is the case in this patient’s treatment.
We understand that Aetna has communicated to the American Chiropractic Association that reimbursement of these two
services is allowed when performed on the same date of service to separate regions if medical necessity is documented.
Therefore, with this information in mind, I have attached a copy of my clinical record for the date(s) of service in question
and the documentation clearly indicates that these services were provided to separate body regions. The documentation
also supports that these services were necessary because:
If you should require additional information specific to this patient or appeal, please feel free to contact me at
Otherwise, please forward payment for the denied services within 30 days.
Sincerely,
Enc: Clinical Record for __________________________________________________________.
 1
1








