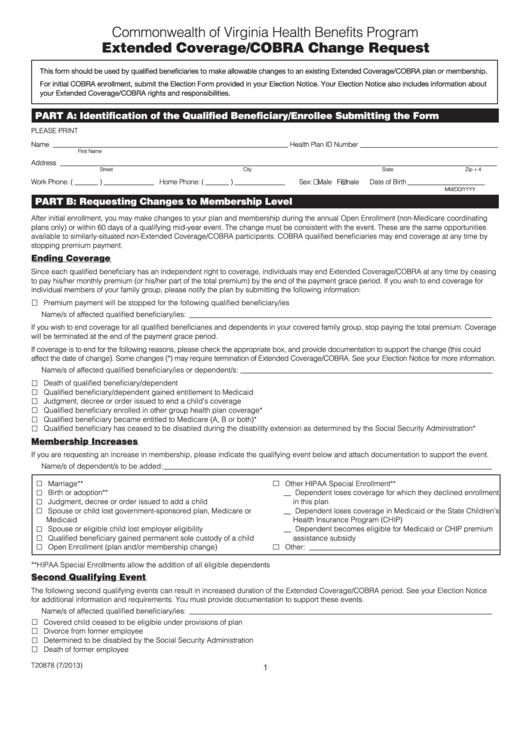
Extended Coverage/cobra Change Request Form-Commonwealth Of Virginia Health Benefits Program
ADVERTISEMENT
Commonwealth of Virginia Health Benefits Program
Extended Coverage/COBRA Change Request
This form should be used by qualified beneficiaries to make allowable changes to an existing Extended Coverage/COBRA plan or membership.
For initial COBRA enrollment, submit the Election Form provided in your Election Notice. Your Election Notice also includes information about
your Extended Coverage/COBRA rights and responsibilities.
PARt A: Identification of the Qualified Beneficiary/Enrollee Submitting the Form
PLEASE PRINT
________________________________________
Name ______________________________________________________________________
Health Plan ID Number
First Name
M.I.
Last Name
______________________________________________________________________________________________________________________
Address
Street
City
State
Zip + 4
Work Phone: ( _______ ) _______________ Home Phone: ( _______ ) _______________
Sex:
Male
Female
Date of Birth _______________________
MM/DD/YYYY
PARt B: Requesting Changes to Membership Level
After initial enrollment, you may make changes to your plan and membership during the annual Open Enrollment (non-Medicare coordinating
plans only) or within 60 days of a qualifying mid-year event. The change must be consistent with the event. These are the same opportunities
available to similarly-situated non-Extended Coverage/COBRA participants. COBRA qualified beneficiaries may end coverage at any time by
stopping premium payment.
Ending Coverage
Since each qualified beneficiary has an independent right to coverage, individuals may end Extended Coverage/COBRA at any time by ceasing
to pay his/her monthly premium (or his/her part of the total premium) by the end of the payment grace period. If you wish to end coverage for
individual members of your family group, please notify the plan by submitting the following information:
Premium payment will be stopped for the following qualified beneficiary/ies
Name/s of affected qualified beneficiary/ies: ___________________________________________________________________________________
If you wish to end coverage for all qualified beneficiaries and dependents in your covered family group, stop paying the total premium. Coverage
will be terminated at the end of the payment grace period.
If coverage is to end for the following reasons, please check the appropriate box, and provide documentation to support the change (this could
affect the date of change). Some changes (*) may require termination of Extended Coverage/COBRA. See your Election Notice for more information.
Name/s of affected qualified beneficiary/ies or dependent/s: _____________________________________________________________________
Death of qualified beneficiary/dependent
Qualified beneficiary/dependent gained entitlement to Medicaid
Judgment, decree or order issued to end a child’s coverage
Qualified beneficiary enrolled in other group health plan coverage*
Qualified beneficiary became entitled to Medicare (A, B or both)*
Qualified beneficiary has ceased to be disabled during the disability extension as determined by the Social Security Administration*
Membership Increases
If you are requesting an increase in membership, please indicate the qualifying event below and attach documentation to support the event.
Name/s of dependent/s to be added: __________________________________________________________________________________________
Marriage**
Other HIPAA Special Enrollment**
Birth or adoption**
__ Dependent loses coverage for which they declined enrollment
Judgment, decree or order issued to add a child
in this plan
Spouse or child lost government-sponsored plan, Medicare or
__ Dependent loses coverage in Medicaid or the State Children’s
Medicaid
Health Insurance Program (CHIP)
Spouse or eligible child lost employer eligibility
__ Dependent becomes eligible for Medicaid or CHIP premium
Qualified beneficiary gained permanent sole custody of a child
assistance subsidy
Open Enrollment (plan and/or membership change)
Other: ____________________________________________________
**HIPAA Special Enrollments allow the addition of all eligible dependents
Second Qualifying Event
The following second qualifying events can result in increased duration of the Extended Coverage/COBRA period. See your Election Notice
for additional information and requirements. You must provide documentation to support these events.
Name/s of affected qualified beneficiary/ies: ___________________________________________________________________________________
Covered child ceased to be eligible under provisions of plan
Divorce from former employee
Determined to be disabled by the Social Security Administration
Death of former employee
T20878 (7/2013)
1
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1 2
2