Sample Of Information For An Initial Treatment Plan Template
ADVERTISEMENT
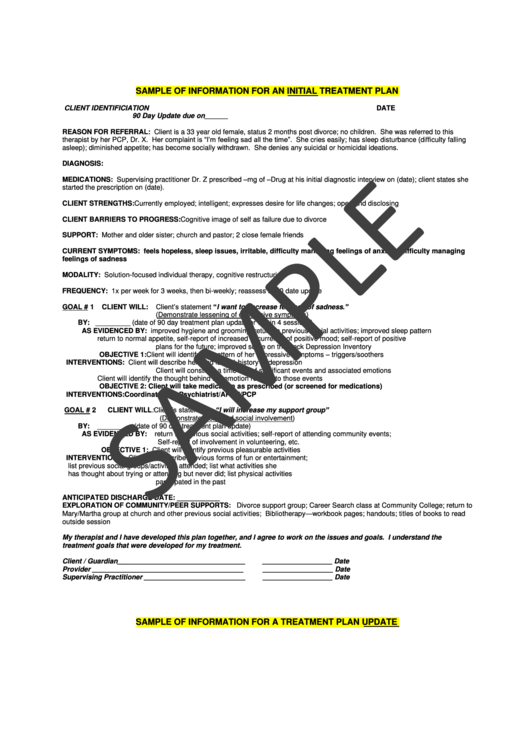
SAMPLE OF INFORMATION FOR AN INITIAL TREATMENT PLAN
CLIENT IDENTIFICIATION
DATE
90 Day Update due on______
REASON FOR REFERRAL: Client is a 33 year old female, status 2 months post divorce; no children. She was referred to this
therapist by her PCP, Dr. X. Her complaint is “I’m feeling sad all the time”. She cries easily; has sleep disturbance (difficulty falling
asleep); diminished appetite; has become socially withdrawn. She denies any suicidal or homicidal ideations.
DIAGNOSIS:
MEDICATIONS: Supervising practitioner Dr. Z prescribed –mg of –Drug at his initial diagnostic interview on (date); client states she
started the prescription on (date).
CLIENT STRENGTHS: Currently employed; intelligent; expresses desire for life changes; open and disclosing
CLIENT BARRIERS TO PROGRESS: Cognitive image of self as failure due to divorce
SUPPORT: Mother and older sister; church and pastor; 2 close female friends
CURRENT SYMPTOMS: feels hopeless, sleep issues, irritable, difficulty managing feelings of anxiety, difficulty managing
feelings of sadness
MODALITY: Solution-focused individual therapy, cognitive restructuring
FREQUENCY: 1x per week for 3 weeks, then bi-weekly; reassess at 90 date update
Client’s statement “I want to decrease feelings of sadness.”
GOAL # 1
CLIENT WILL:
(Demonstrate lessening of depressive symptoms)
BY: _________ (date of 90 day treatment plan update or within 4 sessions)
AS EVIDENCED BY:
improved hygiene and grooming; return to previous social activities; improved sleep pattern
return to normal appetite, self-report of increased occurrence of positive mood; self-report of positive
plans for the future; improved score on the Beck Depression Inventory
OBJECTIVE 1: Client will identify the pattern of her depressive symptoms – triggers/soothers
INTERVENTIONS: Client will describe her (and family) history of depression
Client will construct a time line of significant events and associated emotions
Client will identify the thought behind the emotion relating to those events
OBJECTIVE 2: Client will take medication as prescribed (or screened for medications)
INTERVENTIONS: Coordinate with Psychiatrist/APRN/PCP
CLIENT WILL: Client’s statement “I will increase my support group”
GOAL # 2
(Demonstrate increased social involvement)
BY:
_________ (date of 90 day treatment plan update)
AS EVIDENCED BY:
return to previous social activities; self-report of attending community events;
Self-report of involvement in volunteering, etc.
OBJECTIVE 1: Client will identify previous pleasurable activities
INTERVENTIONS: Client will describe previous forms of fun or entertainment;
list previous social groups/activities attended; list what activities she
has thought about trying or attending but never did; list physical activities
participated in the past
ANTICIPATED DISCHARGE DATE: ___________
EXPLORATION OF COMMUNITY/PEER SUPPORTS: Divorce support group; Career Search class at Community College; return to
Mary/Martha group at church and other previous social activities; Bibliotherapy—workbook pages; handouts; titles of books to read
outside session
My therapist and I have developed this plan together, and I agree to work on the issues and goals. I understand the
treatment goals that were developed for my treatment.
Client / Guardian_________________________________
__________________ Date
Provider _______________________________________
__________________ Date
Supervising Practitioner __________________________
__________________ Date
SAMPLE OF INFORMATION FOR A TREATMENT PLAN UPDATE
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1 2
2








