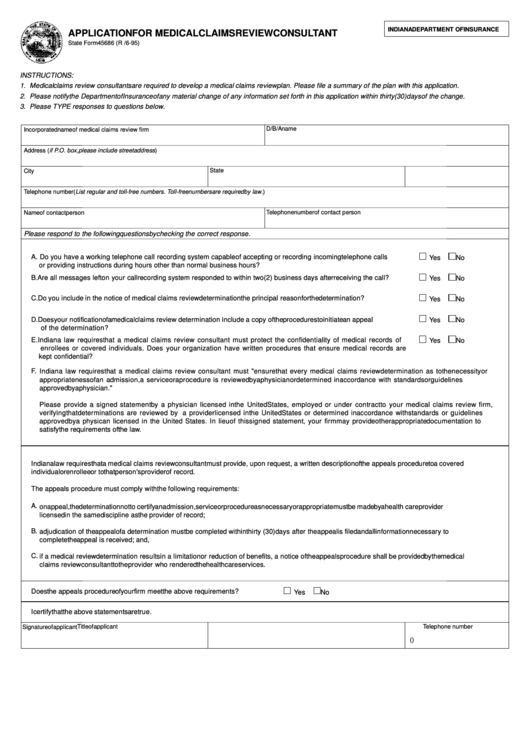
INDIANA DEPARTMENT OF INSURANCE
APPLICATION FOR MEDICAL CLAIMS REVIEW CONSULTANT
State Form 45686 (R / 6-95)
INSTRUCTIONS:
1. Medical claims review consultants are required to develop a medical claims review plan. Please file a summary of the plan with this application.
2. Please notify the Department of Insurance of any material change of any information set forth in this application within thirty (30) days of the change.
3. Please TYPE responses to questions below.
D/B/A name
Incorporated name of medical claims review firm
Address (if P.O. box, please include street address)
State
ZIP code
City
Telephone number (List regular and toll-free numbers. Toll-free numbers are required by law.)
Name of contact person
Telephone number of contact person
Please respond to the following questions by checking the correct response.
A. Do you have a working telephone call recording system capable of accepting or recording incoming telephone calls
Yes
No
or providing instructions during hours other than normal business hours?
B. Are all messages left on your call recording system responded to within two (2) business days after receiving the call?
Yes
No
C. Do you include in the notice of medical claims review determination the principal reason for the determination?
Yes
No
D. Does your notification of a medical claims review determination include a copy of the procedures to initiate an appeal
Yes
No
of the determination?
E. Indiana law requires that a medical claims review consultant must protect the confidentiality of medical records of
Yes
No
enrollees or covered individuals. Does your organization have written procedures that ensure medical records are
kept confidential?
F.
Indiana law requires that a medical claims review consultant must "ensure that every medical claims review determination as to the necessity or
appropriateness of an admission, a service or a procedure is reviewed by a physician or determined in accordance with standards or guidelines
approved by a physician."
Please provide a signed statement by a physician licensed in the United States, employed or under contract to your medical claims review firm,
verifying that determinations are reviewed by a provider licensed in the United States or determined in accordance with standards or guidelines
approved by a physican licensed in the United States. In lieu of this signed statement, your firm may provide other appropriate documentation to
satisfy the requirements of the law.
Indiana law requires that a medical claims review consultant must provide, upon request, a written description of the appeals procedure to a covered
individual or enrollee or to that person's provider of record.
The appeals procedure must comply with the following requirements:
A.
on appeal, the determination not to certify an admission, service or procedure as necessary or appropriate must be made by a health care provider
licensed in the same discipline as the provider of record;
B.
adjudication of the appeal of a determination must be completed within thirty (30) days after the appeal is filed and all information necessary to
complete the appeal is received; and,
C.
if a medical review determination results in a limitation or reduction of benefits, a notice of the appeals procedure shall be provided by the medical
claims review consultant to the provider who rendered the health care services.
Does the appeals procedure of your firm meet the above requirements?
Yes
No
I certify that the above statements are true.
Title of applicant
Telephone number
Signature of applicant
(
)
 1
1