School Health Services Program Manual - General Information - Colorado Department Of Education - Department Of Health Care Policy Page 3
ADVERTISEMENT
School Health Services Program Manual Section 1
Section 1: General Information
The Colorado School Health Services (SHS) Program administered by the
Colorado
Department of Health Care Policy and Financing (the Department)
allows school
districts and Boards of Cooperative Educational Services (BOCES), herein referred to as
“district,” to access federal Medicaid funds for delivering Medicaid allowable school
health services to Medicaid eligible children. Districts may also receive federal funding
through the Medicaid Administrative Claiming (MAC) component for performing
administrative activities which include service coordination, outreach, enrollment and
administrative functions that support the Medicaid program. Reimbursement received
by a district through the SHS Program shall be used by the district to provide additional
and expanded health services.
The SHS Program serves students up to the age of 21 who are eligible under the
provisions of the Individuals with Disabilities Education Act (IDEA) of 1990 as amended
in 2004 and to those enrolled in programs that require an Individualized Education
Program (IEP) or an Individualized Family Services Plan (IFSP). School health services
provided through the SHS Program must be medically necessary (defined in
Section
1.2) and prescribed in the student’s IEP or IFSP.
Program Overview
Participating districts are reimbursed interim payments based on a monthly rate. The
monthly rate is calculated according to each district’s historical Certified Public
Expenditure amounts and paid in twelve equal monthly installments. See Section 4.3 for
additional information on Interim Payments.
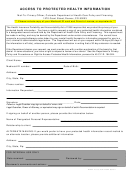
In order to receive interim payments for services, the district documents and submits
Medicaid claims to the Department. The district must first obtain consent from the
parent or guardian of the Medicaid child to bill Medicaid on behalf of the child. The
claim describes the service delivered to the Medicaid child on a specific date, the
medical provider, and additional service information.
See Section 2 for information on Covered Services.
See Section 4.1 and 4.2 for additional information on Claims Requirements
and Claims Submission.
Additionally, the district must participate in a Random Moment Time Study (RMTS) and
cost reporting process. District staff that are Medicaid qualified to provide direct health
services, Targeted Case Management (TCM) or Medicaid administrative activities may
participate in the time study and their eligible costs can be identified in the cost report.
The cost report will determine the Medicaid allowable total costs a district should be
reimbursed.
See Section 3 for additional information on RMTS.
See Section 6 for additional information on MAC- Quarterly Cost Report.
2 |
P a g e
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Legal
 1
1 2
2 3
3 4
4 5
5 6
6 7
7 8
8