Medicaid Ehr Incentive Program Health Information Exchange - Objective Stage 3 - Centers For Medicare And Medicaid Services Page 3
ADVERTISEMENT
Exclusion: Any EP, eligible hospital or CAH for whom the total of transitions or referrals received and patient
encounters in which the provider has never before encountered the patient, is fewer than 100 during the HER
reporting period is excluded from this measure.
NOTE: There are changes to the measure calculations policy, which specifies that actions included the
numerator must occur within the EHR reporting period if that period is a full calendar year, or if it is less than a
full calendar year, within the calendar year in which the EHR reporting period occurs.
Summary of Care Documents
All summary of care documents used to meet this objective must include the information outlined in Table 1 (if
the provider knows it). In circumstances where there is no information available to populate one or more of the
fields listed, either because the provider can be excluded from recording such information or because there is
no information to record (e.g., laboratory tests), the provider may leave the field(s) blank and still meet the
objective and its associated measure.
Note: The current problem list, current medication list, and current medication allergy list may not be left
blank. These fields must include the most recent information known by the EP or eligible hospital as of the time
of generating the summary of care document, or include a notation of no current problem, medication and/or
medication allergies.
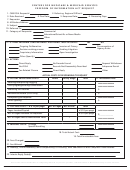
Table 1:
What to Include in Summary of Care Documents
Patient name
Care plan field, including goals and instructions
Referring or transitioning provider's name and
Care team, including the primary care provider of
office contact information (EP only)
record and any additional known care team
Procedures
members beyond the referring or transitioning
Encounter diagnosis
provider and the receiving provider.
Immunizations
Discharge instructions (Hospital Only)
Laboratory test results
Reason for referral (EP only)
Vital signs (height, weight, blood pressure,
BMI)
Summary of care documents must also include:*
Smoking status
Current problem list (providers may also include
Functional status, including activities of daily
historical problems at their discretion)
living, cognitive and disability status
Current medication list (a list of medications that a
Demographic information (preferred
patient is currently taking)
language, sex, race, ethnicity, date of birth)
Current medication allergy list (a list of medications
to which a given patient has known allergies)
* An EP or eligible hospital must verify these three fields for current problem list, current medication list, and
current medication allergy list are not blank and include the most recent information known by the EP or
hospital as of the time of generating the summary of care document
Note about Lab Results: The final rule for Stage 3 requires a provider to have the ability to send all laboratory
test results in the summary of care document. However, the provider may work with their system developer to
establish clinically relevant parameters based on their specialty, patient population, or for certain transitions
and referrals that allow for clinical relevance to determine the most appropriate results for given transition or
3
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1 2
2 3
3 4
4 5
5