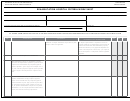
Form Cms-437a - Rehab Unit Criteria Worksheet Page 9
ADVERTISEMENT
THE HOSPITAL REPRESENTATIVE WHO
TAG
REGULATION
GUIDANCE
YES
NO
N/A
COMPLETES THIS ENTIRE FORM
A3523
(4) Has had, after completing a 1 year hospital
• Review personnel and/or credentialing files to
The representative reviews the director of
internship, at least 2 years of training or experience
verify the physician’s training and experience
rehabilitation’s level of training and experience.
in the medical management of inpatients requiring
complies with the regulation.
rehabilitation services.
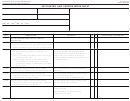
A3524
(h) Have a plan of treatment for each inpatient that
• Conduct a clinical record review to verify that
The representative verifies that the rehab unit has
is established, reviewed, and revised as needed by
each IRF patient has a plan of treatment and
patient plans of treatment.
a physician in consultation with other professional
that the plans are updated whenever there is a
personnel who provide services to the patient.
change in the patient’s condition.
• The plan of treatment should include the
patient’s medical prognosis and the anticipated
interventions, functional outcomes, and
discharge destination from the IRF stay.
• The anticipated interventions detailed in the
overall plan of care should include the expected
intensity (meaning number of hours per day),
frequency (meaning number of days per week),
and duration (meaning total number of days
during the IRF stay) of physical, occupational,
speech-language pathology, and prosthetic/
orthotic therapies required by the patient during
the IRF stay.
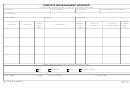
A3525
(i) Use a coordinated interdisciplinary team
• Review clinical records to determine whether the
The representative will determine whether
approach in the rehabilitation of each inpatient,
interdisciplinary team is meeting once a week to
interdiciplinary teams are meeting once weekly to
as documented by the periodic clinical entries
review patient progress toward goal attainment
review patient progress and that documentation is
made in the patient’s medical record to note the
and discharge planning.
in the medical records.
patient’s status in relationship to goal attainment
• Determine if the documentation complies with
and discharge plans and that team conferences
the regulatory requirements.
are held at least once per week to determine the
appropriateness of treatment.
According to the Paperwork Reduction of 1995, no persons are required to respond to a collection of information unless it displays a valid OMB control number. The valid OMB control number for this information collection is 0938-0986. The time required to complete this
information collection is estimated to average 15 minutes per response, including the time to review instructions, search existing data resources, gather the data needed, and complete and review the information collection. If you have any comments concerning the accuracy of the
time estimate(s) or suggestions for improving this form, please write to: CMS, Attn: PRA Reports Clearance Officer, 7500 Security Boulevard, Baltimore, Maryland 21244-1850.
COMMENTS
Form CMS-437A (06/12)
9
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1 2
2 3
3 4
4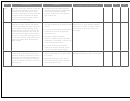 5
5 6
6 7
7 8
8 9
9