Sample Claim File Request
ADVERTISEMENT
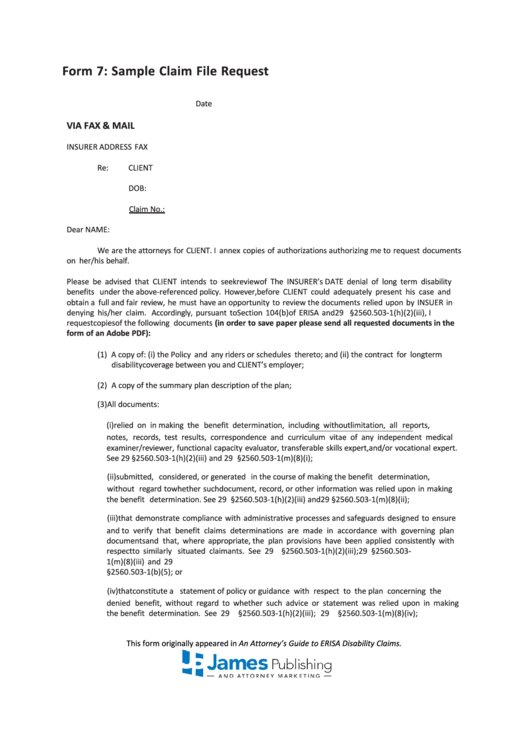
Form 7: Sample Claim File Request
Date
VIA FAX & MAIL
INSURER ADDRESS FAX
Re:
CLIENT
DOB:
Claim No.:
Dear NAME:
We are the attorneys for CLIENT. I annex copies of authorizations authorizing me to request documents
on her/his behalf.
Please be advised that CLIENT intends to seek review of The INSURER’s DATE denial of long term disability
benefits under the above-referenced policy. However, before CLIENT could adequately present his case and
obtain a full and fair review, he must have an opportunity to review the documents relied upon by INSUER in
denying his/her claim. Accordingly, pursuant to Section 104(b) of ERISA and 29 C.F.R. §2560.503-1(h)(2)(iii), I
request copies of the following documents (in order to save paper please send all requested documents in the
form of an Adobe PDF):
(1) A copy of: (i) the Policy and any riders or schedules thereto; and (ii) the contract for long term
disability coverage between you and CLIENT’s employer;
(2) A copy of the summary plan description of the plan;
(3) All documents:
(i) relied on in making the benefit determination, including without limitation, all reports,
notes, records, test results, correspondence and curriculum vitae of any independent medical
examiner/reviewer, functional capacity evaluator, transferable skills expert, and/or vocational expert.
See 29 C.F.R. §2560.503-1(h)(2)(iii) and 29 C.F.R. §2560.503-1(m)(8)(i);
(ii) submitted, considered, or generated in the course of making the benefit determination,
without regard to whether such document, record, or other information was relied upon in making
the benefit determination. See 29 C.F.R. §2560.503-1(h)(2)(iii) and 29 C.F.R. §2560.503-1(m)(8)(ii);
(iii) that demonstrate compliance with administrative processes and safeguards designed to ensure
and to verify that benefit claims determinations are made in accordance with governing plan
documents and that, where appropriate, the plan provisions have been applied consistently with
respect to similarly situated claimants. See 29 C.F.R. §2560.503-1(h)(2)(iii); 29 C.F.R. §2560.503-
1(m)(8)(iii) and 29 C.F.R.
§2560.503-1(b)(5); or
(iv) that constitute a statement of policy or guidance with respect to the plan concerning the
denied benefit, without regard to whether such advice or statement was relied upon in making
the benefit determination. See 29 C.F.R. §2560.503-1(h)(2)(iii); 29 C.F.R. §2560.503-1(m)(8)(iv);
This form originally appeared in An Attorney’s Guide to ERISA Disability Claims.
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Letters
 1
1 2
2 3
3








