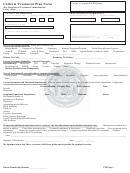
TREATMENT PLAN FORM INSTRUCTIONS
1. Enter the patient’s name in the order of last name, first name, and middle name.
2. Enter the patient's date of birth.
3. Enter the patient’s Medi-Cal number.
4. Enter the primary counselor’s name.
5. Enter the agency’s name.
6. Enter the patient's DSM-5 Diagnosis(es).
7. Answer the question “Is Patient’s Physical Examination Result Available?” If the answer is affirmative, mark the “yes” box; if the physical exam
result is not available mark the “no” box and enter the date of scheduled physical exam appointment.
8. Enter the date the patient assessment was performed.
9. Enter the date the treatment plan is updated.
PROBLEM(S) # 1-4
10. Enter the problem statement. Problem statements focus on the patient’s current areas of concern and their most immediate areas of need.
11. Enter the long-term goal for this problem. Long-term goals are the ultimate results desired when a plan is established or revised.
12. Enter the treatment start date.
13. Enter the relevant ASAM dimension for respective problem.
14. Select severity level for the respective problem (0 for none; 1 for mild, 2 for moderate, 3 for severe, and 4 for very severe).
15. Enter the short-term goal for this problem. Short-term goals can be achieved in a limited period of time and frequently lead to the achievement of a
long-term goal. Short-term goal(s) must be SMART: Specific, Measurable, Attainable within the treatment plan review period, Realistic, and
Time-bound. SMART goals must be linked to the patient’s functional impairment and diagnosis, as documented in the assessment. Multiple short-term
goals should be prioritized numerically (1, 2, 3, etc).
16. Enter the action steps that will be implemented to achieve the correlated short-term goal. Multiple action steps should be prioritized sequentially
(1a, 1b, 1c, etc).
17. Enter the projected target date for the patient to achieve the correlated short-term goal(s).
18. Enter the completion date the patient actually achieved the short-term goal(s).
19. Mark the type and frequency of services to be provided to the patient. (“x week” means the number of times the marked service will be provided to
the patient per week).
Additionally, indicate if the patient is referred for Medication-Assisted Treatment (MAT) and provide the reasons why patient is referred or not
referred (e.g., opioid user, patient is already on MAT, patient declined, etc.).
NAME AND SIGNATURE OF INVOLVED PARTIES
20. Enter the patient’s signature.
21. Enter the date the patient signs the treatment plan.
22. Mark “Not Applicable’ if patient’s signature is present. If the required patient signature is absent, provide explanation of the refusal or unavailability
of the patient signature and document the plan to engage the patient to participate in treatment plan development/updates.
23. Enter the counselor’s name.
24. Enter the counselor’s signature.
25. Enter the date the counselor signs the treatment plan.
26. Enter the LPHA’s name.
*Note: Licensed Practitioner of the Healing Arts [LPHA] includes Physicians, Nurse Practitioners, Physician Assistants, Registered Nurses, Registered
Pharmacists, Licensed Clinical Psychologists [LCP], Licensed Clinical Social Workers [LCSW], Licensed Professional Clinical Counselors [LPCC],
and Licensed Marriage and Family Therapists [LMFT] and licensed-eligible practitioners working under the supervision of licensed clinicians.
27. Enter the LPHA’s signature.
28. Enter the date the LPHA reviews and signs the treatment plan.
TREATMENT PLAN REVIEW
29. Enter the date the counselor/LPHA reviewed the treatment plan.
30. Enter the date for the progress note that documents details of treatment plan review.
31. Enter additional comments, if applicable.
32. Enter the counselor/LPHA’s name.
33. Enter the counselor/LPHA’s signature.
SUBMIT THE TREATMENT PLAN FORM TO:
Mail:
Substance Abuse Prevention and Control
1000 S. Fremont Ave., Bldg. A9 East, 3rd Floor
Alhambra, CA 91803
Fax:
(XXX) XXX-XXXX
Website:
3
Treatment Plan Form
Revised 5/13/2016
 1
1 2
2 3
3 4
4