Patient Health History Form
ADVERTISEMENT
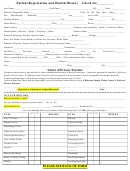
PATIENT HEALTH HISTORY FORM
Patient Name: _______________________________________
Birth date: ____/____/____ Date: ____/____/_____
Primary Care Physician: _____________________________ ____
City: ______________________________________
Reason for today’s visit:
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
CURRENT/PRIOR ILLNESSES/INJURIES
PAST SURGERIES
Please list ALL medications (prescription and non- prescription) that you take. (Include herbal remedies, vitamins, over-
the-counter, street drugs, prescriptions etc.)
MEDICATION
DOSAGE
MEDICATION
DOSAGE
Do you take any blood thinning products such as Vitamin E, Plavix, Coumadin, or Aspirin?
NO
YES
Do you have any food, environmental, or drug allergies?
NO
YES
(Please explain below)
ALLERGY
TYPE
REACTION
Do you smoke?
NO and Never have
YES
(Please explain below)
TYPE OF SMOKING
HOW MUCH
HOW LONG
(cigarette, pipe marijuana, chew, etc.)
Do you drink alcohol?
NO and Never have
Socially Only
Daily
Beer/ Wine
Hard Liquor
Occupation: ____________________________________________________________________________
Please describe any family health issue below:
FAMILY HISTORY
GOOD/ NONE
UNKNOWN
ILLNESSES/ REASON FOR DEATH
MOTHER
FATHER
SIBLING(S)
OTHER HEREDITARY ILLNESS
Patient Signature: __________________________________________ Date: ____/_____/_____
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1 2
2