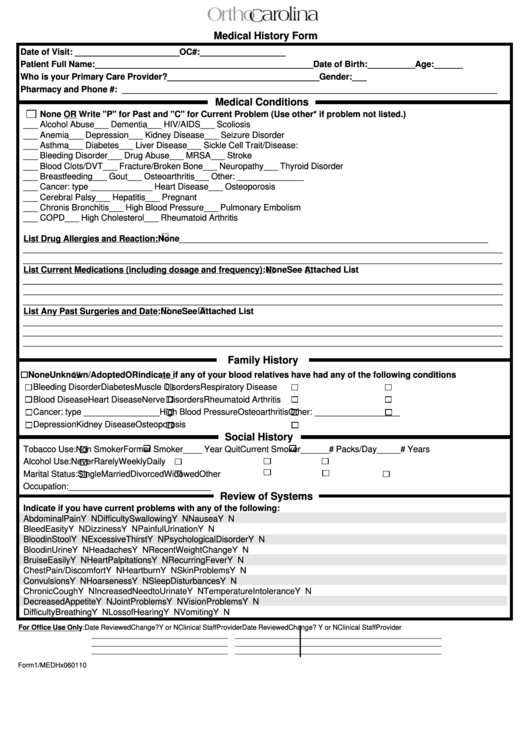
Medical History Form
ADVERTISEMENT
Medical History Form
Date of Visit: ______________________
OC#: __________________
Patient Full Name: ______________________________________________
Date of Birth: __________
Age: ______
Who is your Primary Care Provider? ________________________________ Gender: ___
Pharmacy and Phone #: _______________________________________________________________________________
Medical Conditions
None OR Write "P" for Past and "C" for Current Problem (Use other* if problem not listed.)
___ Alcohol Abuse
___ Dementia
___ HIV/AIDS
___ Scoliosis
___ Anemia
___ Depression
___ Kidney Disease
___ Seizure Disorder
___ Asthma
___ Diabetes
___ Liver Disease
___ Sickle Cell Trait/Disease:
___ Bleeding Disorder
___ Drug Abuse
___ MRSA
___ Stroke
___ Blood Clots/DVT
___ Fracture/Broken Bone
___ Neuropathy
___ Thyroid Disorder
___ Breastfeeding
___ Gout
___ Osteoarthritis
___ Other: ______________
___ Cancer: type __________ ___ Heart Disease
___ Osteoporosis
___ Cerebral Palsy
___ Hepatitis
___ Pregnant
___ Chronis Bronchitis
___ High Blood Pressure
___ Pulmonary Embolism
___ COPD
___ High Cholesterol
___ Rheumatoid Arthritis
List Drug Allergies and Reaction:
None _________________________________________________________________
_____________________________________________________________________________________________________
_____________________________________________________________________________________________________
List Current Medications (including dosage and frequency):
None
See Attached List
_____________________________________________________________________________________________________
_____________________________________________________________________________________________________
_____________________________________________________________________________________________________
List Any Past Surgeries and Date:
None
See Attached List
_____________________________________________________________________________________________________
_____________________________________________________________________________________________________
_____________________________________________________________________________________________________
Family History
None
Unknown/Adopted OR indicate if any of your blood relatives have had any of the following conditions
Bleeding Disorder
Diabetes
Muscle Disorders
Respiratory Disease
Blood Disease
Heart Disease
Nerve Disorders
Rheumatoid Arthritis
Cancer: type ________________
High Blood Pressure
Osteoarthritis
Other: __________________
Depression
Kidney Disease
Osteoporosis
Social History
Tobacco Use:
Non Smoker
Former Smoker ____ Year Quit
Current Smoker______# Packs/Day _____# Years
Alcohol Use:
Never
Rarely
Weekly
Daily
Marital Status:
Single
Married
Divorced
Widowed
Other
Occupation:______________________________
Review of Systems
Indicate if you have current problems with any of the following:
Abdominal Pain
Y N
Difficulty Swallowing
Y N
Nausea
Y N
Bleed Easity
Y N
Dizziness
Y N
Painful Urination
Y N
Blood in Stool
Y N
Excessive Thirst
Y N
Psychological Disorder
Y N
Blood in Urine
Y N
Headaches
Y N
Recent Weight Change
Y N
Bruise Easily
Y N
Heart Palpitations
Y N
Recurring Fever
Y N
Chest Pain / Discomfort
Y N
Heartburn
Y N
Skin Problems
Y N
Convulsions
Y N
Hoarseness
Y N
Sleep Disturbances
Y N
Chronic Cough
Y N
Increased Need to Urinate
Y N
Temperature Intolerance Y N
Decreased Appetite
Y N
Joint Problems
Y N
Vision Problems
Y N
Difficulty Breathing
Y N
Loss of Hearing
Y N
Vomiting
Y N
For Office Use Only:
Date Reviewed
Change? Y or N
Clinical Staff
Provider
Date Reviewed
Change? Y or N
Clinical Staff
Provider
____________
_____________
__________ _________
____________
____________
__________
__________
____________
_____________
__________ _________
____________
____________
__________
__________
____________
_____________
__________ _________
____________
____________
__________
__________
Form1/MEDHx060110
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1








