Employer Notice Of Election - Healthpass Page 3
ADVERTISEMENT
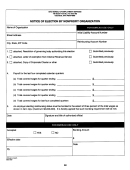
F. BANK INFORMATION
An electronic payment or business check, payable to HealthPass, for the full amount due must accompany this application. Applications submitted with less than the full amount
due or with personal checks will not be processed.
For the initial payment, how do you prefer to pay for your coverage? (Select One)
Please use electronic funds transfer (EFT) for my initial payment with HealthPass.
r
(Must attach a voided business check)
I have remitted a physical check with my application.
r
Are any COBRA members included in the first month’s premium? rYes rNo
After the initial payment, how do you prefer to pay for your coverage? (Select One)
Please use electronic funds transfer (EFT) for my monthly payment.
r
(Must attach a voided business check)
Please bill me monthly.
r
If selected, I hereby authorize HealthPass to initiate electronic funds transfer (EFT) from my account for the payment of my monthly cost of coverage. I understand the debit transaction
will occur the first (1st) of the month or the first (1st) business day following. In the event that I make changes to my banking arrangements, I understand that I must notify HealthPass to
effect the changes for payment collection. All changes must be reported 20 days prior to the effective date of the change by calling HealthPass at 888.313.7277.
G. EMPLOYER CERTIFICATION
I agree and attest that:
My business will offer HealthPass medical coverage to every eligible full-time employee and age, sex or health status cannot be used to determine employee eligibility.
l
An eligible employee must be defined as one that works no less than 20 hours per week and my business must have at least one (1) such eligible employee.
l
Part-time employees (working under 20 hours per week), temporary or seasonal employees, consultants and independent contractors (1099’s), household help,
l
and retirees are not eligible for coverage through HealthPass. Other exclusions may apply.
75% of eligible employees must elect to participate in HealthPass medical coverage or have other credible health insurance coverage.
l
The HealthPass coverage area is New York, New Jersey, Connecticut, and Bucks County, PA. If 75% or less of the eligible employees live outside of the coverage
l
area, then all out-of-coverage area employees can be covered through HealthPass. If more than 75% of the eligible employees live outside of the coverage area, they
must be considered ineligible for the group to participate. Specific restrictions on plan availability by carrier may apply.
This application has been completed with accurate information and has in no way has any information been misrepresented, falsely provided, or reinforced by false
l
documentation that has been presented. Any person who, knowingly and with intent to defraud any insurance company or other person, files an application for
insurance or state department of claim containing any materially false information, or conceals for the purpose of misleading, information concerning any fact material
there to, commits a fraudulent insurance act, which is a crime, and shall also be subject to civil penalty not to exceed $5,000 and the stated value of the claim for
each such violation plus the amount of the claim on individuals who commit fraudulent insurance acts. Additionally, the State has the right to levy a civil fine of up to
$1,000 for possession of a fraudulent health insurance identification card and up to $5,000 for each addition card possessed.
Please refer to our Eligibility Guidelines for more detailed information.
H. MEDICARE SECONDARY PAYER
The Medicare Secondary Payer (MSP) provisions apply to situations when Medicare is not the primary payer. If your company has employed 19 or fewer employees in the
current or preceding year, Medicare is almost always primary. If your company has employed 20 or more employees in the current or preceding year, Medicare is almost
always secondary. In the case where an employer has 19 or fewer employees and is part of a multi-employer group health plan (e.g. HealthPass) then Medicare is by
default the secondary payer to the group health plan (GHP).
Participating employers with HealthPass that certify they have 19 or fewer employees, and have enrolling employees age 65 or older, must file for the MSP Small Employer
Exception Certification. The exception means the employer is not held to the MSP rules governing multi-employer group health plans and Medicare will be the primary payer of
Medicare Part A claims for any employee that is a working-aged Medicare beneficiary.
For purposes of this calculation both full-time and part-time employees are counted toward the 20 employee threshold. Self-employed individuals participating in a GHP are not counted as employees for
purposes of determining if the 20 or more employee requirement is met. The 20 employee or more requirement is met if the employer employed 20 or more employees for each working day in each of 20
or more calendar weeks in the current or preceding year. Note that the 20 weeks do not have to be consecutive. An employer is considered to have 20 or more employees for each working day of a
particular week if the employer has at least 20 full and/or part-time employees on its employment rolls each working day of that week.
r My group size per Medicare standards:* _______
If your answer is 20 or more, no further action needs to be taken. If your answer is 19 or fewer and you have at least one enrolling employee age 65+, you must complete and sign the MSP Small Employer
Exception Certification ( ) and return it with this application.
I. PROGRAM BENEFITS
TM
Health Advocate: All members with medical coverage through HealthPass (excluding COBRA enrollees) have access to Health Advocate
to assist with navigating
many healthcare related issues, including support in understanding claims and accessing providers.
Section 125 POP Kit: All groups enrolled with HealthPass have access to a Section 125 Premium Only Plan (POP) Kit which enables employees to make pre-tax
contributions to their healthcare rates. Employers must request their POP Kit within 90 days of enrollment by visiting
HealthPass COBRA Administration Services: All groups have access to COBRA/NYSC Administration Services unless opted out by Employer in Section C.
The service includes notification of former employees of their rights upon termination and the collection of payments from employees who elect to continue their coverage
with their former employer. Employer understands it is responsible to timely and accurately perform all of their responsibilities by providing participant information as
outlined at HealthPass COBRA Administration Services will terminate if (i) mandatory termination occurs due to non-payment or Employer otherwise
ceases to offer medical insurance via HealthPass; (ii) Employer does not comply with the information outlined at
or; (iii) Employer elects to cease to offer
HealthPass COBRA Administration Services by declining such services in Section C of this form or otherwise in writing at any time. Employer agrees to indemnify HealthPass
and all personnel involved in the provision of COBRA Administration Services.
TM
Medical Cost Advocate: All members have access to Medical Cost Advocate
to help negotiate incurred out of pocket costs with providers on their behalf
(additional fees may apply).
Visit
for further information on the Program Benefits.
Page 3 of 4
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Legal
 1
1 2
2 3
3 4
4