Employer Notice Of Election - Healthpass Page 4
ADVERTISEMENT
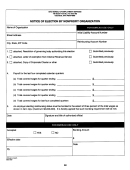
J. FEE DISCLOSURE
Program Fees: All medical rates include $4.95 for HealthPass Program Benefits (non-carrier/agent services) and a 2.9% billing and administrative fee.
l Guardian PPO plans: EE $9.25, EE/Spouse $18.25, EE+Child(ren) $16.50, Family $26.50
l EverGuard and EverGuard Plus plans: $3.50 Per Employee Per Month (PEPM)
l VisionGuard: $1.50 PEPM
l Solstice PPO: EE $9.25, EE/Spouse $18.25, EE+Child(ren) $16.50, Family $26.50
l Solstice Vision: $1.50
K. HEALTHPASS INSURANCE TRUST
The undersigned employer, in order to establish a plan or plans of Group Health Insurance for its employees and their dependents, hereby requests participation in
the New York Health Purchasing Alliance, Inc. HealthPass Insurance Trust (the “Trust”) which provides health insurance benefits under Group Contracts issued by
several health insurers and health maintenance organizations (HMO) to the Trustee of the HealthPass Insurance Trust. If the undersigned employer’s participation is
approved by the Trustee or the Administrator appointed by the Trustee (the “Administrator”), said employer shall become a Participating Employer (as defined in
Trust Agreement) as of the effective date endorsed herein by the Trustee or the Administrator. The undersigned employer understands and acknowledges that even
if it is approved as a Participating Employer in the HealthPass Insurance Trust, its employees and their dependents are not automatically insured, but must each
satisfy any eligibility requirements of the Trust and of the applicable Group Contracts. The employer agrees to make the coverage under Group Contracts available
to all of its current and future eligible employees.
The undersigned employer hereby agrees:
l To be bound by all the terms of the Trust Agreement and of the Group Contract(s) as each may be from time to time amended, changed or terminated by the
Insurer, HMO or Trustee, copies of which are available from the Trust or the Administrator upon request.
l To furnish any information requested by the Trustee, Administrator or any of the Insurers or HMOs, which is reasonably required for the proper administration of
the Trust or of the Group Contract.
l To distribute to its eligible employees any materials provided by or on behalf of the Trustee, Administrator, Health Insurer or HMO describing Trust or the Group Contract.
l That it has no right, title or interest in or to the Trust Fund created under Trust.
l Coverage under any Contract through the Trust shall only apply to the extent provided in the Group Contract issued to the Trust by the insurer or HMO. All
claims for benefits must be submitted to the insurer or HMO. Benefits are payable only by the insurer or HMO. The Trust’s responsibility is solely to pay premiums
to the insurer or HMO. The Trust is not liable for any benefit payments.
l The Trustee does not have any obligation under any of the Group Contracts to automatically insure employer groups should HealthPass not be in receipt of the
premium by the end of the month of the date due. Full payment must be made to keep all group policies active.
L. EMPLOYER AUTHORIZATION
IN WITNESS hereof, the Employer, by its duly authorized officer, certifies the Employer:
r Meets the eligibility requirements including, but not limited to, the criteria specified in Section G,
r Has completed Sections A, B and H with accurate information and have in no way misrepresented, falsely provided, or reinforced any information with false documentation,
r Authorizes any initial and ongoing payments as specified in Section F,
r Understands and agrees to the requirements of the Program Benefits afforded in Section I and the related fees as enumerated in Section J, and;
r Agrees to the terms set forth in Section K of this form regarding the Trust Participation Agreement.
Moreover, the Employer, by its duly authorized officer, understands that all enrollment documentation must be fully complete and submitted by the 20th of the month
prior for effective coverage for the 1st of the following month. Any enrollment documentation received after the 20th of the month will subject the entire group to delays in
coverage activation up to 10-12 business days.
Authorized Signature _______________________________________
Title ______________________________________
Print Name _________________________________________________
Date______________________________________
Page 4 of 4
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Legal
 1
1 2
2 3
3 4
4