NOTIFICATION OF RIGHT TO CONTINUE GROUP HEALTH COVERAGE
Qualifying Events and Continuation Period
To be eligible for continuation coverage, an employee must have been insured under the employer’s
PacificSource group health insurance policy for at least the last three continuous months, and the member must
experience a qualifying event that causes a loss of coverage under the terms of the group health insurance policy.
If your employer changed health insurance plans or carriers during that time without a break in coverage and you
were enrolled in your employer’s plan continuously for the last three months, you will be eligible. An employee
that has been covered under the employer’s policy for less than three months, or has had a break in coverage
during the last three months is not eligible for continuation.
Each covered person (employee/subscriber) or qualified beneficiary (employee, spouse, or dependent child) may
elect continuation together or separately.
Qualifying Event
Continuation Period
Employee’s termination of employment or
Employee, spouse, and children may continue for up to nine
reduction in hours
months
Employee’s divorce
Spouse and children may continue for up to nine months
Employee’s eligibility for Medicare benefits
Spouse and children may continue for up to nine months
Employee’s death
Spouse and children may continue for up to nine months
Child no longer qualifies as a dependent
Child may continue for up to nine months
When Coverage Ends
Your continuation coverage will end before the end of the nine-month maximum continuation period listed above if
any of the following occurs:
• Your continuation premium is not paid on time;
• You become covered under another group health plan;
• You become eligible for Medicare benefits;
• The group discontinues its health plan and no longer offers a group health plan to any of its employees.
Plan Changes or Termination
While it does not currently intend to do so, your employer has the right to change the benefits of its health plan or
eliminate the plan entirely. If that happens, any changes to the group health plan will also apply to everyone
enrolled in continuation coverage. If your employer terminates the health plan, your continuation coverage will
also terminate.
Enrollment Deadline
To continue coverage, this form must reach PacificSource within 31 days after your last day of coverage under
the group policy, or within 10 days after you receive notification of your continuation rights, whichever is later. If
your continuation election form is not returned by the deadline, your coverage will end on the last day you were
eligible under the group health policy.
Dependent Coverage
To include your eligible dependents, you must list your family members in Section 4 on page 1 of this form. If your
dependents were not covered prior to the qualifying event, they may not enroll in the continuation coverage at this
time. Only newborn or adopted children may enroll in the continuation coverage after the qualifying event.
Premium Payments for Continued Coverage
The cost of continuation coverage is your responsibility. You must pay your premium to your former employer
before the first day of each month for which you want coverage. The employer will include your continuation
premium with the group’s monthly payment to PacificSource. PacificSource cannot accept premium directly from
you. If your premium is not paid on time, your coverage will end. If your coverage is cancelled due to a missed
payment, it will not be reinstated for any reason. Premium rates are established annually and may be adjusted if
the plan’s benefits or costs change.
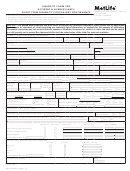
Group Coverage Continuation Election Form OR 1014
 1
1 2
2 3
3