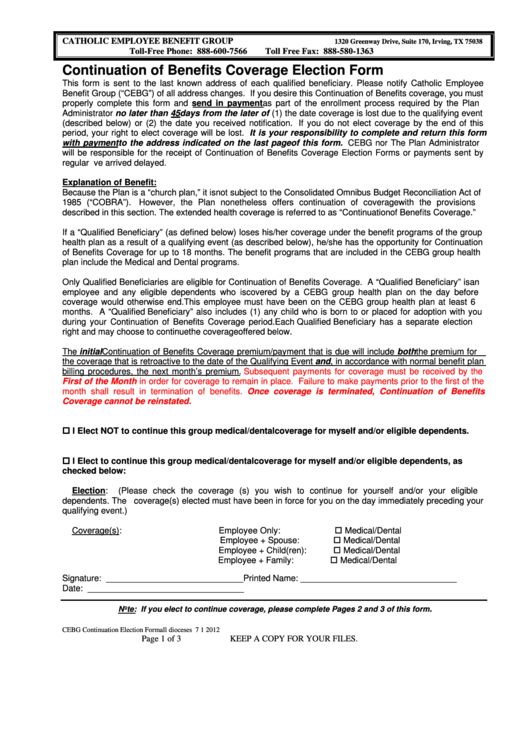
Continuation Of Benefits Coverage Election Form
ADVERTISEMENT
CATHOLIC EMPLOYEE BENEFIT GROUP
1320 Greenway Drive, Suite 170, Irving, TX 75038
Toll-Free Phone: 888-600-7566
Toll Free Fax: 888-580-1363
Continuation of Benefits Coverage Election Form
This form is sent to the last known address of each qualified beneficiary. Please notify Catholic Employee
Benefit Group (“CEBG”) of all address changes. If you desire this Continuation of Benefits coverage, you must
properly complete this form and send in payment as part of the enrollment process required by the Plan
Administrator no later than 45 days from the later of (1) the date coverage is lost due to the qualifying event
(described below) or (2) the date you received notification. If you do not elect coverage by the end of this
period, your right to elect coverage will be lost. It is your responsibility to complete and return this form
with payment to the address indicated on the last page of this form. CEBG nor The Plan Administrator
will be responsible for the receipt of Continuation of Benefits Coverage Election Forms or payments sent by
regular U.S. mail that have arrived delayed.
Explanation of Benefit:
Because the Plan is a “church plan,” it is not subject to the Consolidated Omnibus Budget Reconciliation Act of
1985 (“COBRA”).
However, the Plan nonetheless offers continuation of coverage with the provisions
described in this section. The extended health coverage is referred to as “Continuation of Benefits Coverage.”
If a “Qualified Beneficiary” (as defined below) loses his/her coverage under the benefit programs of the group
health plan as a result of a qualifying event (as described below), he/she has the opportunity for Continuation
of Benefits Coverage for up to 18 months. The benefit programs that are included in the CEBG group health
plan include the Medical and Dental programs.
Only Qualified Beneficiaries are eligible for Continuation of Benefits Coverage. A “Qualified Beneficiary” is an
employee and any eligible dependents who is covered by a CEBG group health plan on the day before
coverage would otherwise end. This employee must have been on the CEBG group health plan at least 6
months. A “Qualified Beneficiary” also includes (1) any child who is born to or placed for adoption with you
during your Continuation of Benefits Coverage period. Each Qualified Beneficiary has a separate election
right and may choose to continue the coverage offered below.
The initial Continuation of Benefits Coverage premium/payment that is due will include both the premium for
the coverage that is retroactive to the date of the Qualifying Event and, in accordance with normal benefit plan
billing procedures, the next month’s premium.
Subsequent payments for coverage must be received by the
First of the Month in order for coverage to remain in place. Failure to make payments prior to the first of the
month shall result in termination of benefits. Once coverage is terminated, Continuation of Benefits
Coverage cannot be reinstated.
I Elect NOT to continue this group medical/dental coverage for myself and/or eligible dependents.
I Elect to continue this group medical/dental coverage for myself and/or eligible dependents, as
checked below:
Election:
(Please check the coverage (s) you wish to continue for yourself and/or your eligible
dependents. The coverage(s) elected must have been in force for you on the day immediately preceding your
qualifying event.)
Medical/Dental
Coverage(s):
Employee Only:
Medical/Dental
Employee + Spouse:
Medical/Dental
Employee + Child(ren):
Medical/Dental
Employee + Family:
Signature: _____________________________ Printed Name: _________________________________
Date: _________________________________
.
Note: If you elect to continue coverage, please complete Pages 2 and 3 of this form
CEBG Continuation Election Form all dioceses 7 1 2012
Page 1 of 3
KEEP A COPY FOR YOUR FILES.
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1 2
2 3
3








