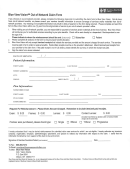
Out Of Network Claim Form Page 2
ADVERTISEMENT
DMC
THIS FORM CAN BE USED FOR DMC CARE OUT-OF-NETWORK MEDICAL, BH/SA, OR PHARMACY CLAIMS.
FOR OUT-OF-NETWORK MEDICAL CLAIMS
EMPLOYEES:
1.
You must complete this form for each different illness or accident. Fill out the top two sections (PATIENT INFORMATION
& EMPLOYEE INFORMATION).
2.
Attach an itemized receipt from the out-of-network medical provider.
3.
If the out-of-network provider (physician, hospital, physical therapist, etc.) is billing directly, have the provider complete the
claim form and return it to DMC CARE Claims Department.
4.
Payments for services will be sent to the subscriber unless the provider is billing directly for services.
5.
DMC CARE members, please call (800) 543-0161 for further information.
HEALTH CARE PROVIDERS:
1.
Complete the bottom portion of the form. Payment will be made directly to you unless your statement shows payment was
made by the member. Hospitals use the UB-92 or your standard itemized billing form.
2.
Providers can call (800) 543-0161 to verify eligibility, benefits coverage, claim inquiries, or obtain authorization.
MAIL ALL OUT-OF-NETWORK MEDICAL CLAIM FORMS AND ITEMIZED RECEIPTS TO:
DMC CARE CLAIMS DEPARTMENT
P. O. BOX 44290
DETROIT, MI 48244
FOR OUT-OF-NETWORK BEHAVIORAL HEALTH AND SUBSTANCE ABUSE CLAIMS
EMPLOYEES:
1.
Fill out the top two sections (PATIENT INFORMATION & EMPLOYEE INFORMATION).
2.
Attach an itemized receipt from the out-of-network provider.
3.
If the out-of-network provider (physician, hospital, therapist, etc.) is billing directly, have the provider complete the claim
form and return it to Value Options.
4.
Payment for services will be sent to the subscriber unless the provider is billing directly for services.
5.
DMC CARE PPO members, please call (877) 362-2472 (DMC-BHSA) for further information.
HEALTH CARE PROVIDERS:
1.
Complete the bottom portion of the form. Payment will be made directly to you unless your statement shows payment was
made by the member. Hospitals use the UB-92 or your standard itemized billing form.
2.
Providers can call (877) 362-2472 (DMC-BHSA) to verify eligibility, benefits coverage, claim inquiries or obtain authorization.
MAIL ALL OUT-OF-NETWORK BEHAVIORAL HEALTH OR SUBSTANCE ABUSE CLAIMS TO:
VALUE OPTIONS
ATTN: CLAIMS DEPARTMENT
ONE TOWNE SQUARE, SUITE 600
SOUTHFIELD, MI 48076
FOR OUT-OF-NETWORK PRESCRIPTION DRUG CLAIMS
EMPLOYEES:
1.
Fill out the top two sections (PATIENT INFORMATION & EMPLOYEE INFORMATION)
2.
Attach an itemized receipt from the out-of-network pharmacy. The receipt must include the following information:
•
Pharmacy Name and Address
•
Member’s Name
•
Prescription Dispensing Date
•
Units Dispensed
•
Drug Name
•
11 digit National Drug Code (available from the pharmacist)
•
Days supplied
•
Amount Paid by DMC CARE Member
3.
All payments for services will be sent directly to the employee.
4.
Pharmacies or DMC CARE members, please call (877) 647-4026 for further information.
MAIL ALL OUT-OF-NETWORK PRESCRIPTION DRUG CLAIM FORMS AND ITEMIZED RECEIPTS TO:
4D PHARMACY MANAGEMENT SYSTEMS, INC.
300 NORTH OLD WOODWARD
BIRMINGHAM, MI 48009
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Legal
 1
1 2
2