Post-Service Appeals Form - Njm
ADVERTISEMENT
NJM
N
J
M
I
C
Insurance
EW
ERSEY
ANUFACTURERS
NSURANCE
OMPANY
Group
301 Sullivan Way, West Trenton, NJ 08628
609-883-1300 /
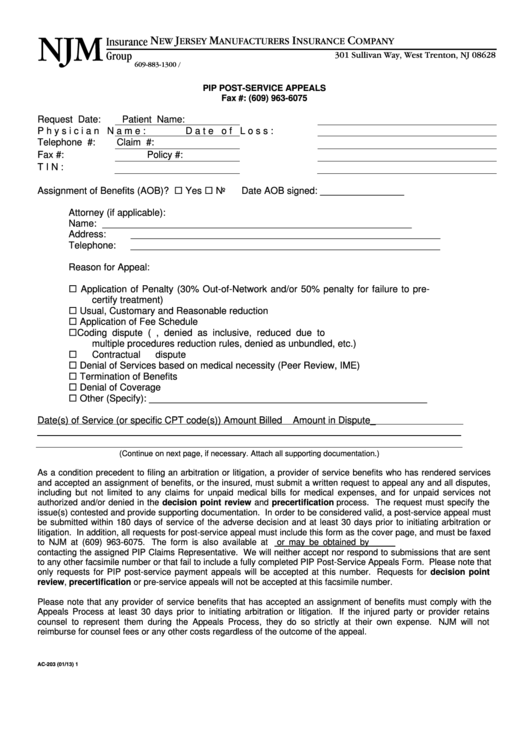
PIP POST-SERVICE APPEALS
Fax #: (609) 963-6075
Request Date:
Patient Name:
Physician Name:
Date of Loss:
Telephone #:
Claim #:
Fax #:
Policy #:
TIN:
Assignment of Benefits (AOB)? Yes
No
Date AOB signed: ________________
Attorney (if applicable):
Name:
___________________________________________________________
Address:
___________________________________________________________
Telephone:
___________________________________________________________
Reason for Appeal:
Application of Penalty (30% Out-of-Network and/or 50% penalty for failure to pre-
certify treatment)
Usual, Customary and Reasonable reduction
Application of Fee Schedule
Coding dispute (e.g. denied as incorrect, denied as inclusive, reduced due to
multiple procedures reduction rules, denied as unbundled, etc.)
Contractual dispute
Denial of Services based on medical necessity (Peer Review, IME)
Termination of Benefits
Denial of Coverage
Other (Specify): _____________________________________________________
Date(s) of Service (or specific CPT code(s))
Amount Billed
Amount in Dispute_
________________________________________________________________________________
(Continue on next page, if necessary. Attach all supporting documentation.)
As a condition precedent to filing an arbitration or litigation, a provider of service benefits who has rendered services
and accepted an assignment of benefits, or the insured, must submit a written request to appeal any and all disputes,
including but not limited to any claims for unpaid medical bills for medical expenses, and for unpaid services not
authorized and/or denied in the decision point review and precertification process. The request must specify the
issue(s) contested and provide supporting documentation. In order to be considered valid, a post-service appeal must
be submitted within 180 days of service of the adverse decision and at least 30 days prior to initiating arbitration or
litigation. In addition, all requests for post-service appeal must include this form as the cover page, and must be faxed
to NJM at (609) 963-6075. The form is also available at or may be obtained by
contacting the assigned PIP Claims Representative. We will neither accept nor respond to submissions that are sent
to any other facsimile number or that fail to include a fully completed PIP Post-Service Appeals Form. Please note that
only requests for PIP post-service payment appeals will be accepted at this number. Requests for decision point
review, precertification or pre-service appeals will not be accepted at this facsimile number.
Please note that any provider of service benefits that has accepted an assignment of benefits must comply with the
Appeals Process at least 30 days prior to initiating arbitration or litigation. If the injured party or provider retains
counsel to represent them during the Appeals Process, they do so strictly at their own expense. NJM will not
reimburse for counsel fees or any other costs regardless of the outcome of the appeal.
AC-203 (01/13)
1
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Legal
 1
1 2
2








