Patient Care Report
ADVERTISEMENT
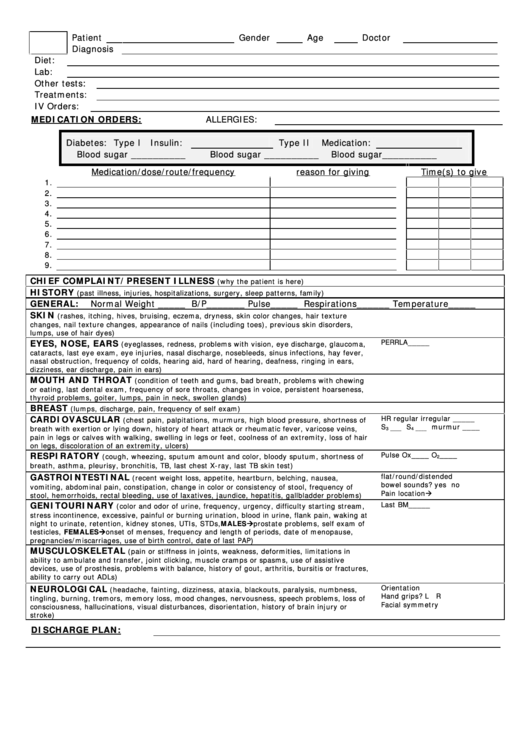
Patient
Gender
Age
Doctor
Diagnosis
Diet:
Lab:
Other tests:
Treatments:
IV Orders:
MEDICATION ORDERS:
ALLERGIES:
Diabetes: Type I
Insulin:
Type II
Medication:
Blood sugar __________
Blood sugar __________
Blood sugar__________
Medication/dose/route/frequency
reason for giving
Time(s) to give
1.
2.
3.
4.
5.
6.
7.
8.
9.
CHIEF COMPLAINT/PRESENT ILLNESS
(why the patient is here)
HISTORY
(past illness, injuries, hospitalizations, surgery, sleep patterns, family)
GENERAL:
Normal Weight _____ B/P_______ Pulse_____ Respirations______ Temperature_____
SKIN
(rashes, itching, hives, bruising, eczema, dryness, skin color changes, hair texture
changes, nail texture changes, appearance of nails (including toes), previous skin disorders,
lumps, use of hair dyes)
EYES, NOSE, EARS
PERRLA_____
(eyeglasses, redness, problems with vision, eye discharge, glaucoma,
cataracts, last eye exam, eye injuries, nasal discharge, nosebleeds, sinus infections, hay fever,
nasal obstruction, frequency of colds, hearing aid, hard of hearing, deafness, ringing in ears,
dizziness, ear discharge, pain in ears)
MOUTH AND THROAT
(condition of teeth and gums, bad breath, problems with chewing
or eating, last dental exam, frequency of sore throats, changes in voice, persistent hoarseness,
thyroid problems, goiter, lumps, pain in neck, swollen glands)
BREAST
(lumps, discharge, pain, frequency of self exam)
CARDIOVASCULAR
HR regular irregular _____
(chest pain, palpitations, murmurs, high blood pressure, shortness of
S
S
murmur ____
breath with exertion or lying down, history of heart attack or rheumatic fever, varicose veins,
3 ____
4 ____
pain in legs or calves with walking, swelling in legs or feet, coolness of an extremity, loss of hair
on legs, discoloration of an extremity, ulcers)
RESPIRATORY
Pulse Ox____ O
____
(cough, wheezing, sputum amount and color, bloody sputum, shortness of
2
breath, asthma, pleurisy, bronchitis, TB, last chest X-ray, last TB skin test)
GASTROINTESTINAL
flat/round/distended
(recent weight loss, appetite, heartburn, belching, nausea,
bowel sounds? yes no
vomiting, abdominal pain, constipation, change in color or consistency of stool, frequency of
Pain location
stool, hemorrhoids, rectal bleeding, use of laxatives, jaundice, hepatitis, gallbladder problems)
GENITOURINARY
Last BM_____
(color and odor of urine, frequency, urgency, difficulty starting stream,
stress incontinence, excessive, painful or burning urination, blood in urine, flank pain, waking at
night to urinate, retention, kidney stones, UTIs, STDs, MALESprostate problems, self exam of
testicles, FEMALESonset of menses, frequency and length of periods, date of menopause,
pregnancies/miscarriages, use of birth control, date of last PAP)
MUSCULOSKELETAL
(pain or stiffness in joints, weakness, deformities, limitations in
ability to ambulate and transfer, joint clicking, muscle cramps or spasms, use of assistive
devices, use of prosthesis, problems with balance, history of gout, arthritis, bursitis or fractures,
ability to carry out ADLs)
NEUROLOGICAL
Orientation
(headache, fainting, dizziness, ataxia, blackouts, paralysis, numbness,
Hand grips? L R
tingling, burning, tremors, memory loss, mood changes, nervousness, speech problems, loss of
Facial symmetry
consciousness, hallucinations, visual disturbances, disorientation, history of brain injury or
stroke)
DISCHARGE PLAN:
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1