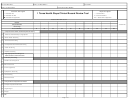
Chart Review Tool Page 2
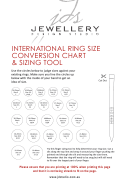
ADVERTISEMENT
C
C
H
H
A
A
R
R
T
T
R
R
E
E
V
V
I
I
E
E
W
W
T
T
O
O
O
O
L
L
County of Los Angeles – Department of Mental Health
REQUIREMENT
FINDING
CORRECTIVE ACTION PLAN
ASSESSMENT (A)
8. If client is identified as Non-English speaking in the Assessment, is there
Yes
No
documentation showing that services were provided in his/her preferred language in
English is Primary
the Client Care Plan and/or Progress Notes?
Language
9. Other than language, if cultural considerations (e.g., cultural identity, client’s cultural
Yes
No
explanation of his/her illness, role of religion/spirituality in providing support) or
No cultural considerations
special service needs (e.g., hearing impaired, blind, access issues) were identified
identified
in the Assessment, is there documentation showing that services addressed these
issues in the Client Care Plan and/or Progress Note?
10. Medical Necessity: Is there an “Included” Diagnosis?
Yes
No
Yes
No
*
11.
Medical Necessity: Are impairments in life functioning and their relationship to
the client’s symptoms/behaviors documented?
AMHD Initials: _____
If No to #10 or #11, claiming must be immediately discontinued and services not claimed to Medi-Cal.
CLIENT CARE / COORDINATION PLAN (CCCP)
Not Required per:
Episode will be closed prior to intake/review period
Other (please specify)_______________________
12. Is there a completed CCCP for the period being reviewed?
Yes
No
If No to #12, complete and date at next client contact. Please Note: A Client Care Plan should be in place when treatment is provided within 30- or 60-day period
Yes
No
*
13.
Are the objectives in the CCCP related to the symptoms/behaviors or impairments
that are identified in the Assessment?
AMHD Initials: _____
If No to #13, staff must be required to correct the disconnect immediately (i.e., add to Assessment, rewrite/add objective to CCCP)
14. Is there a SMART (specific, measureable, attainable, realistic, and time bound)
Yes
No
objective associated with each type of service provided or expected to be provided?
15. a. Are there specific interventions and modality (e.g. individual therapy, group
Yes
No
rehab) identified for the types of services checked (e.g., MHS, TCM, MSS)?
Yes
No
b. Is the frequency of each type of service documented?
16. Is there an AMHD signature present for all objectives?
Yes
No
Yes
No
17. For medication support objectives, is there a MD, DO, and/or NP signature present?
18. Is documentation legible?
Yes
No
19. a. Has the client/representative signed the CCCP?
Yes
No
Yes
No
b. If not, is there regular documentation of attempts to obtain signature?
If No to #16, #17, #18 and/or #19, claiming must be immediately discontinued until signature(s) and/or appropriate / legible documentation is in place.
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1 2
2 3
3 4
4