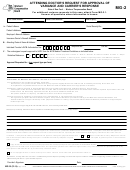
TO THE CARRIER/EMPLOYER/SELF-INSURED EMPLOYER/SPECIAL FUND
Response Time and Notification Required:
The carrier/employer/self-insured employer/Special Fund must approve or grant each variance request in writing by completing this form
and sending it by fax or email to the Treating Medical Provider, claimant's legal counsel, if any, any parties of interest, and the Workers'
Compensation Board. The carrier/ employer/self-insured employer/Special Fund may respond orally to the Treating Medical Provider about
the variance requested by such provider. If the insurance carrier or Special Fund responds orally, it still must send a written response
within the appropriate time period. If the carrier submits a notice of an IME or Medical Records Review within 5 business days of the
variance request, the carrier has 30 calendar days to get the IME exam or Medical Records Review and submit Form IME-4. If no notice of
an IME or Medical Record Review is submitted, the carrier has 15 calendar days from the date of the request to reply to the variance
request.
Denial of the Variance Request:
For a denial of a variance request for medical treatment, the carrier/employer/self-insured employer/Special Fund must explain why it was
denied and attach the written report of the medical professional--a physician, registered physician assistant, registered professional nurse,
or nurse practitioner licensed by New York State, or the appropriate state where the professional practices, who is employed by an
insurance carrier or Special Fund, or has been directly retained by the insurance carrier or Special Fund or is employed by a URAC
accredited company retained by the insurance carrier or Special Fund through a contract to review claims and advise the insurance carrier
or Special Fund--that reviewed the variance request. Such report shall include a list describing the medical records reviewed by the
medical professional when considering the variance request. The carrier has the option to submit citations or copies of relevant literature
published in recognized, peer-reviewed medical journals in support of a denial of a variance request. A medical report supporting the denial
of the variance request is not necessary when the denial is based upon the allegation that (1) the provider did not meet the burden of proof
that a variance is appropriate, (2) the medical care for which the variance is requested has already been rendered, (3) the medical care
requested is not covered under Section 13(a) of the Workers' Compensation Law, (4) the claimant did not appear for a scheduled
independent medical examination, or (5) a new variance request was submitted prior to a substantially similar request being granted or
denied or a substantially similar variance request has been denied, and the resubmitted request does not contain any additional
documentation or justification.
Controverted Claims:
If the compensation case is controverted, the carrier/self-insured employer/employer/Special Fund must still respond to the variance
request timely and in the same manner as requests in non-controverted claims. If the carrier/employer/self-insured employer/Special Fund
approves a variance request when a claim is controverted or the compensability of the body part is controverted, the approval only relates
to medical necessity and shall not be construed as an admission that the condition for which variance is requested is compensable. The
carrier/employer/self-insured employer/Special Fund shall not be responsible for the payment of medical care which is the subject of the
variance request until the question of compensability is resolved.
Failure to Timely Respond to Variance
Report:
A valid variance may be deemed approved by an Order of the Chair issued by the Workers' Compensation Board if the carrier/employer/
self-insured employer/Special Fund
fails to respond to a properly completed request within the time frames specified
above. The
Order of the Chair is the final decision of the Board.
MG-2.0 (12-14)
 1
1 2
2 3
3 4
4