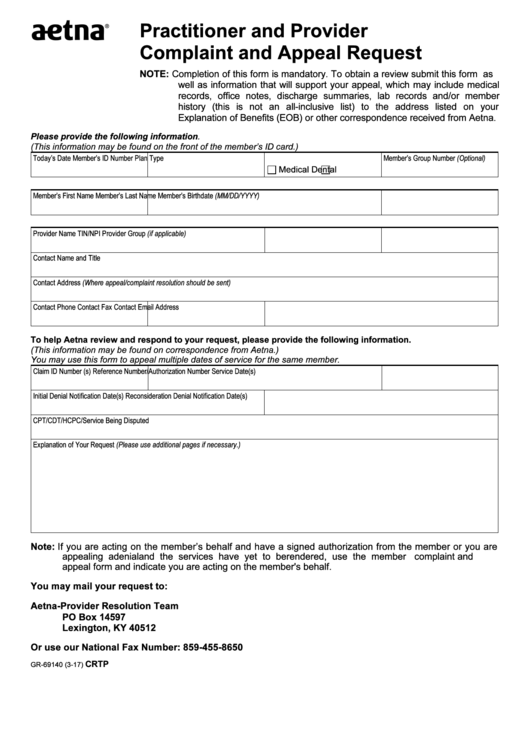
Practitioner and Provider
Complaint and Appeal Request
NOTE: Completion of this form is mandatory. To obtain a review submit this form as
well as information that will support your appeal, which may include medical
records, office notes, discharge summaries, lab records and/or member
history (this is not an all-inclusive list) to the address listed on your
Explanation of Benefits (EOB) or other correspondence received from Aetna.
Please provide the following information.
(This information may be found on the front of the member’s ID card.)
Today’s Date
Member’s ID Number
Plan Type
Member’s Group Number (Optional)
Medical
Dental
Member’s First Name
Member’s Last Name
Member’s Birthdate (MM/DD/YYYY)
Provider Name
TIN/NPI
Provider Group (if applicable)
Contact Name and Title
Contact Address (Where appeal/complaint resolution should be sent)
Contact Phone
Contact Fax
Contact Email Address
To help Aetna review and respond to your request, please provide the following information.
(This information may be found on correspondence from Aetna.)
You may use this form to appeal multiple dates of service for the same member.
Claim ID Number (s)
Reference Number/Authorization Number
Service Date(s)
Initial Denial Notification Date(s)
Reconsideration Denial Notification Date(s)
CPT/CDT/HCPC/Service Being Disputed
Explanation of Your Request (Please use additional pages if necessary.)
Note: If you are acting on the member’s behalf and have a signed authorization from the member or you are
appealing a denial and the services have yet to be rendered, use the member complaint and
appeal form and indicate you are acting on the member's behalf.
You may mail your request to:
Aetna-Provider Resolution Team
PO Box 14597
Lexington, KY 40512
Or use our National Fax Number: 859-455-8650
GR-69140 (3-17)
CRTP
 1
1








