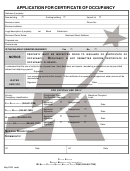
City Of New York Employee Benefits Program Continuation Of Coverage Application Page 8
ADVERTISEMENT
Notice
Under the law you have sixty (60) days from the date you receive this notice to elect continuation
coverage for your City basic and/or optional benefits. Contact your welfare fund administrator for further
instructions on how to continue your welfare fund benefits. Payments of the initial monthly premium may
accompany the enclosed Continuation of Coverage Application opting for continuation. However, under the
law you have a grace period of 45 days from the date you applied for COBRA coverage to pay the premium.
You will receive a partial bill for any remaining portion of the following calendar month to bring your billing
date to the first of the month. All subsequent bills will be charged from the first day of the month during your
COBRA continuation period. Payment shall be on a monthly basis. There is a 30-day grace period for
subsequent late payments.
If you choose COBRA continuation coverage, and you are not Medicare-eligible, the City is required to
offer you the same coverage which is provided to similarly situated employees, retirees or family members.
The law requires that you be afforded the opportunity to maintain continuation coverage for a maximum of
thirty-six (36) months unless you lost coverage because of a termination of employment or reduction in
hours. In the latter case, the required continuation coverage period is a maximum of 18 months. The
maximum period of continuation begins on the first day of the month following the month in which the initial
qualifying event occurred, regardless of when any additional events may take place. However, the law also
provides that your continuation of coverage may be cut short for any of the following reasons:
1)
The premium for continuation coverage is not paid in a timely fashion;
2)
The continuation enrollee becomes covered as an employee or dependent under another
group health or welfare plan (under this occurrence the spouse and dependents may
continue their COBRA coverage for the remaining months of eligibility).
NOTE: If the new plan contains any exclusion or limitation for a pre-existing condition of the continuation
enrollee, then coverage may not be terminated.
You do not have to show that you are insurable to choose continuation coverage. However, under
the law, you have to pay 102% of the cost of benefits for the continuation coverage. Also, at the end of the
continuation period you are allowed to convert to a self-paid direct payment policy.
Conversion Options
If you do not choose continuation, your City group coverage will end. You will still be offered the
opportunity to convert your City health insurance benefits to a non-City direct payment health insurance
policy and, where applicable, convert certain welfare fund benefits. Benefits offered under the non-City group
direct payment health insurance policy are offered on a quarterly basis for an indefinite period of time,
provided premiums are paid on time. These benefits may vary from the City's "basic" health benefits package
in terms of scope of benefits and cost. Benefits available from welfare funds that may be converted to direct
payment are insured medical/ surgical/ hospital and life insurance coverage. Such benefits
may
be
converted within 45 days of termination of coverage.
In order to receive continuation coverage for welfare fund benefits or to convert to direct payment,
you must contact your welfare fund directly.
For further information about this law, employees should contact their agency benefits representative
and retirees should contact the Health Benefits Program, 40 Rector Street - 3rd Fl., New York, New York
10006.
4
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Legal
 1
1 2
2 3
3 4
4 5
5 6
6 7
7 8
8