Claim Correction Form
Download a blank fillable Claim Correction Form in PDF format just by clicking the "DOWNLOAD PDF" button.
Open the file in any PDF-viewing software. Adobe Reader or any alternative for Windows or MacOS are required to access and complete fillable content.
Complete Claim Correction Form with your personal data - all interactive fields are highlighted in places where you should type, access drop-down lists or select multiple-choice options.
Some fillable PDF-files have the option of saving the completed form that contains your own data for later use or sending it out straight away.
ADVERTISEMENT
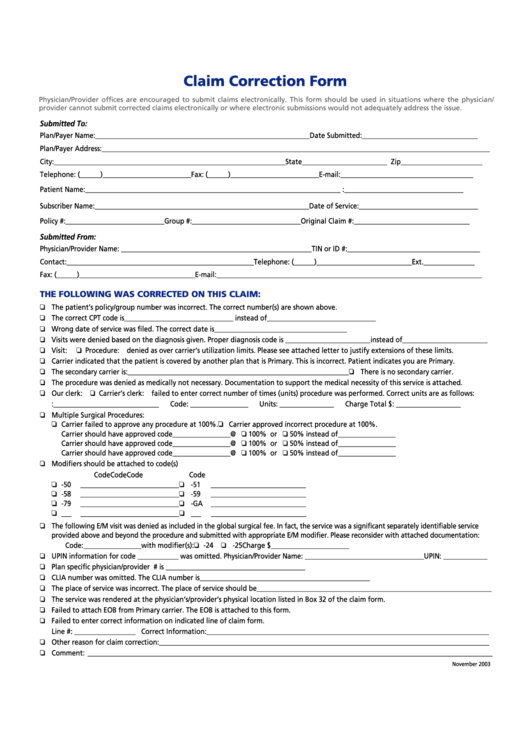
Claim Correction Form
Physician/Provider offices are encouraged to submit claims electronically. This form should be used in situations where the physician/
provider cannot submit corrected claims electronically or where electronic submissions would not adequately address the issue.
Submitted To:
Plan/Payer Name: _______________________________________________________________
Date Submitted: __________________________________
Plan/Payer Address: __________________________________________________________________________________________________________________
City: ____________________________________________________________________ State _________________________ Zip ________________________
Telephone: (______) __________________________ Fax: (______) __________________________ E-mail: _______________________________________
Patient Name: ___________________________________________________________________________ D.OB.: ___________________________________
First
M.I.
Last
Subscriber Name: _______________________________________________________________
Date of Service: ___________________________________
Policy #: _____________________________ Group #: ________________________________
Original Claim #: __________________________________
Submitted From:
Physician/Provider Name: ________________________________________________________
TIN or ID #: _______________________________________
Contact: _______________________________________________________ Telephone: (______) ____________________________ Ext. _______________
Fax: (______) __________________________________ E-mail: ______________________________________________________________________________
THE FOLLOWING WAS CORRECTED ON THIS CLAIM:
The patient’s policy/group number was incorrect. The correct number(s) are shown above.
The correct CPT code is ________________________________ instead of ________________________________
Wrong date of service was filed. The correct date is _______________________________________
Visits were denied based on the diagnosis given. Proper diagnosis code is _________________________ instead of _________________________
Visit:
Procedure: denied as over carrier’s utilization limits. Please see attached letter to justify extensions of these limits.
Carrier indicated that the patient is covered by another plan that is Primary. This is incorrect. Patient indicates you are Primary.
The secondary carrier is: _________________________________________________________________
There is no secondary carrier.
The procedure was denied as medically not necessary. Documentation to support the medical necessity of this service is attached.
Our clerk:
Carrier’s clerk: failed to enter correct number of times (units) procedure was performed. Correct units are as follows:
D.O.S.: _______________________________
Code: _________________
Units: ________________
Charge Total $: ___________________
Multiple Surgical Procedures:
Carrier failed to approve any procedure at 100%.
Carrier approved incorrect procedure at 100%.
Carrier should have approved code _________________ @
100% or
50% instead of _________________
Carrier should have approved code _________________ @
100% or
50% instead of _________________
Carrier should have approved code _________________ @
100% or
50% instead of _________________
Modifiers should be attached to code(s)
Code
Code
Code
Code
-50
______________
_______________
-51
______________
______________
-58
______________
_______________
-59
______________
______________
-79
______________
_______________
-GA
______________
______________
___
______________
_______________
___
______________
______________
The following E/M visit was denied as included in the global surgical fee. In fact, the service was a significant separately identifiable service
provided above and beyond the procedure and submitted with appropriate E/M modifier. Please reconsider with attached documentation:
Code: _________________
with modifier(s):
-24
-25
Charge $ _______________________
UPIN information for code ____________ was omitted. Physician/Provider Name: ___________________________________ UPIN: _____________
Plan specific physician/provider I.D. omitted. The I.D. # is _________________________________________
CLIA number was omitted. The CLIA number is __________________________________________________
The place of service was incorrect. The place of service should be _____________________________________________________________________
The service was rendered at the physician’s/provider’s physical location listed in Box 32 of the claim form.
Failed to attach EOB from Primary carrier. The EOB is attached to this form.
Failed to enter correct information on indicated line of claim form.
Line #: __________________ Correct Information: ___________________________________________________________________________________
Other reason for claim correction: _________________________________________________________________________________________________
Comment: _______________________________________________________________________________________________________________________
November 2003
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Legal
 1
1








