Appeal Request Form
Download a blank fillable Appeal Request Form in PDF format just by clicking the "DOWNLOAD PDF" button.
Open the file in any PDF-viewing software. Adobe Reader or any alternative for Windows or MacOS are required to access and complete fillable content.
Complete Appeal Request Form with your personal data - all interactive fields are highlighted in places where you should type, access drop-down lists or select multiple-choice options.
Some fillable PDF-files have the option of saving the completed form that contains your own data for later use or sending it out straight away.
ADVERTISEMENT
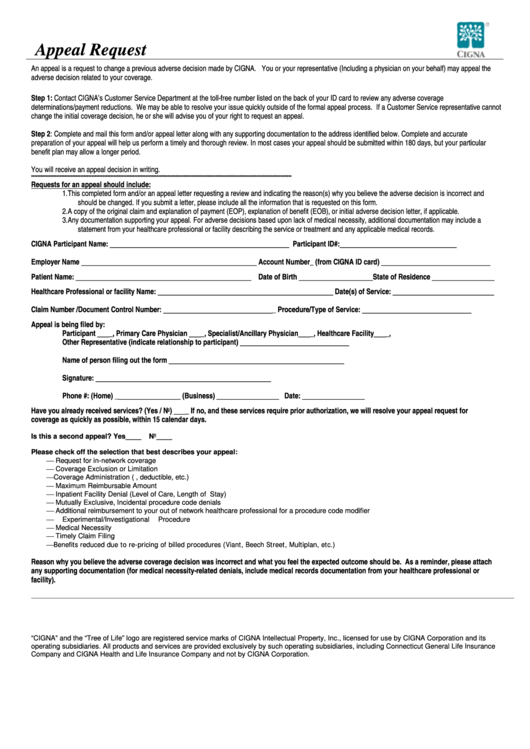
Appeal Request
An appeal is a request to change a previous adverse decision made by CIGNA. You or your representative (Including a physician on your behalf) may appeal the
adverse decision related to your coverage.
Step 1: Contact CIGNA’s Customer Service Department at the toll-free number listed on the back of your ID card to review any adverse coverage
determinations/payment reductions. We may be able to resolve your issue quickly outside of the formal appeal process. If a Customer Service representative cannot
change the initial coverage decision, he or she will advise you of your right to request an appeal.
Step 2: Complete and mail this form and/or appeal letter along with any supporting documentation to the address identified below. Complete and accurate
preparation of your appeal will help us perform a timely and thorough review. In most cases your appeal should be submitted within 180 days, but your particular
benefit plan may allow a longer period.
You will receive an appeal decision in writing.
********************************************************************************************************************************************************************
Requests for an appeal should include:
1.
This completed form and/or an appeal letter requesting a review and indicating the reason(s) why you believe the adverse decision is incorrect and
should be changed. If you submit a letter, please include all the information that is requested on this form.
2.
A copy of the original claim and explanation of payment (EOP), explanation of benefit (EOB), or initial adverse decision letter, if applicable.
3.
Any documentation supporting your appeal. For adverse decisions based upon lack of medical necessity, additional documentation may include a
statement from your healthcare professional or facility describing the service or treatment and any applicable medical records.
CIGNA Participant Name:
Participant ID#:
______________________________________________
______________________________
Employer Name
Account Number_ (from CIGNA ID card)
_____________________________________________
____________________________
Patient Name:
Date of Birth
State of Residence
_____________________________________________
___________________
________________
Healthcare Professional or facility Name:
Date(s) of Service:
_____________________________________________
__________________________
Claim Number /Document Control Number:
_ Procedure/Type of Service:
____________________________
____________________________
Appeal is being filed by:
Participant
_, Primary Care Physician
_, Specialist/Ancillary Physician
_, Healthcare Facility
_,
___
___
___
___
Other Representative (indicate relationship to participant)
____________________________
Name of person filing out the form
_____________________________________________
Signature:
_____________________________________________
Phone #: (Home) _
(Business)
Date:
________________
________________
________________
Have you already received services? (Yes / No)
_ If no, and these services require prior authorization, we will resolve your appeal request for
___
coverage as quickly as possible, within 15 calendar days.
Is this a second appeal? Yes____
No____
Please check off the selection that best describes your appeal:
⎯
Request for in-network coverage
⎯
Coverage Exclusion or Limitation
⎯
Coverage Administration (i.e. co-pay, deductible, etc.)
⎯
Maximum Reimbursable Amount
⎯
Inpatient Facility Denial (Level of Care, Length of Stay)
⎯
Mutually Exclusive, Incidental procedure code denials
⎯
Additional reimbursement to your out of network healthcare professional for a procedure code modifier
⎯
Experimental/Investigational Procedure
⎯
Medical Necessity
⎯
Timely Claim Filing
⎯
Benefits reduced due to re-pricing of billed procedures (Viant, Beech Street, Multiplan, etc.)
Reason why you believe the adverse coverage decision was incorrect and what you feel the expected outcome should be. As a reminder, please attach
any supporting documentation (for medical necessity-related denials, include medical records documentation from your healthcare professional or
facility).
_____________________________________________________________________________________________________________________________________________________________________________________________________
“CIGNA” and the “Tree of Life” logo are registered service marks of CIGNA Intellectual Property, Inc., licensed for use by CIGNA Corporation and its
operating subsidiaries. All products and services are provided exclusively by such operating subsidiaries, including Connecticut General Life Insurance
Company and CIGNA Health and Life Insurance Company and not by CIGNA Corporation.
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Business
 1
1 2
2








