An Employer'S Guide To Group Health Continuation Coverage Under Cobra - Employee Benefits Security Administration - U.s. Department Of Labor Page 13
ADVERTISEMENT
Second Qualifying Event
An 18-month extension may be available to qualified beneficiaries receiving an 18-month maximum period of continuation
coverage (giving a total maximum period of 36 months of continuation coverage) if the qualified beneficiaries experience
a second qualifying event that is death of the covered employee, divorce or legal separation of the covered employee and
spouse, Medicare entitlement (in certain circumstances), or loss of dependent child status under the plan. The second event
can be a second qualifying event only if it would have caused the qualified beneficiary to lose coverage under the plan in
the absence of the first qualifying event.
The plan must have procedures for how a qualified beneficiary should provide notice of a second qualifying event. These
rules should be described in the plan’s SPD (and in the election notice for any offer of an 18-month period of continuation
coverage). The plan can set a time limit for providing this notice, but the time limit cannot be shorter than 60 days from
the latest of: (1) the date on which the qualifying event occurs; (2) the date on which the qualified beneficiary loses (or
would lose) coverage under the plan as a result of the qualifying event; or (3) the date on which the qualified beneficiary
is informed, through the furnishing of either the SPD or the COBRA general notice, of the responsibility to notify the plan
and the procedures for doing so.
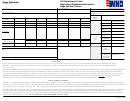
Summary of Qualifying Events, Qualified Beneficiaries, and
Maximum Periods of Continuation Coverage
The following chart shows the maximum period for which continuation coverage must be offered for the specific qualifying
events and the qualified beneficiaries who are entitled to elect continuation coverage when the specific event occurs. Note
that an event is a qualifying event only if it causes the qualified beneficiary to lose coverage under the plan.
MAXIMUM PERIOD OF
QUALIFIED
CONTINUATION
QUALIFYING EVENT
BENEFICIARIES
COVERAGE
Termination (for reasons other than gross
Employee
18 months
3
misconduct) or reduction in hours of employment
Spouse
Dependent Child
Employee enrollment in Medicare
Spouse
36 months
4
Dependent Child
Divorce or legal separation
Spouse
36 months
Dependent Child
Death of employee
Spouse
36 months
Dependent Child
Loss of “dependent child” status under the plan
Dependent Child
36 months
In certain circumstances, qualified beneficiaries entitled to 18 months of continuation coverage may become entitled to a disability extension of an additional 11
3
months (for a total maximum of 29 months) or an extension of an additional 18 months due to the occurrence of a second qualifying event (for a total maximum
of 36 months). (See Duration of Continuation Coverage earlier in this booklet.)
The actual period of continuation coverage may vary depending on factors such as whether the Medicare entitlement occurred prior to or after the end of the
4
covered employee’s employment or reduction in hours. For more information, see Duration of Continuation Coverage earlier in this booklet or contact
askebsa.dol.gov or by calling 1-866-444-3272.
the Department of Labor’s Employee Benefits Security Administration (EBSA) electronically at
9
AN EMPLOYER’S GUIDE TO GROUP HEALTH CONTINUATION COVERAGE UNDER COBRA
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Letters
 1
1 2
2 3
3 4
4 5
5 6
6 7
7 8
8 9
9 10
10 11
11 12
12 13
13 14
14 15
15 16
16 17
17 18
18 19
19