An Employer'S Guide To Group Health Continuation Coverage Under Cobra - Employee Benefits Security Administration - U.s. Department Of Labor Page 8
ADVERTISEMENT
COBRA Notice and Election Procedures
Under COBRA, group health plans must provide covered employees and their families with specific notices explaining
their COBRA rights. Plans must also have rules for how COBRA continuation coverage is offered, how qualified
beneficiaries may elect continuation coverage, and when it can be terminated.
Notice Procedures
Summary Plan Description
The COBRA rights provided under the plan, like other important plan information, must be described in the plan’s
Summary Plan Description (SPD). The SPD is a written document that gives important information about the plan,
including what benefits are available under the plan, the rights of participants and beneficiaries under the plan, and how
the plan works. ERISA requires group health plans to give each participant an SPD within 90 days after he or she first
becomes a participant in a plan (or within 120 days after the plan is first subject to the reporting and disclosure provisions
of ERISA). In addition, if there are material changes to the plan, the plan must give participants a Summary of Material
Modifications (SMM) not later than 210 days after the end of the plan year in which the changes become effective. If the
change is a material reduction in covered services or benefits, the SMM must be furnished not later than 60 days after the
reduction is adopted. A participant or beneficiary covered under the plan may request a copy of the SPD and any SMMs
(as well as any other plan documents), which must be provided within 30 days of a written request.
COBRA General Notice
Group health plans must give each employee and each spouse of an employee who becomes covered under the plan a
general notice describing COBRA rights. The general notice must be provided within the first 90 days of coverage. Group
health plans can satisfy this requirement by including the general notice in the plan’s SPD and giving the SPD to the
employee and to the spouse within this time limit.
The general notice must include:
•
The name of the plan and the name, address, and telephone number of someone whom the employee and spouse
can contact for more information on COBRA and the plan;
•
A general description of the continuation coverage provided under the plan;
•
An explanation of what qualified beneficiaries must do to notify the plan of qualifying events or disabilities;
•
An explanation of the importance of keeping the plan administrator informed of addresses of the participants and
beneficiaries; and
•
A statement that the general notice does not fully describe COBRA or the plan and that more complete
information is available from the plan administrator and in the SPD.
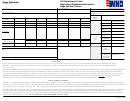
The Department of Labor has developed a model general notice that single-employer group health plans may use to satisfy
the general notice requirement. It is available at dol.gov/ebsa. In order to use this model general notice properly, the
plan administrator must complete it by filling in the blanks with the appropriate plan information. Use of the model general
notice, appropriately completed, will be considered by the Department to be good faith compliance with the general notice
content requirements of COBRA.
4
UNITED STATES DEPARTMENT OF LABOR
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Letters
 1
1 2
2 3
3 4
4 5
5 6
6 7
7 8
8 9
9 10
10 11
11 12
12 13
13 14
14 15
15 16
16 17
17 18
18 19
19