The Merit-Based Incentive Payment System: Mips Scoring Methodology Overview - Centers For Medicare & Medicaid Services Page 45
ADVERTISEMENT
Identify MIPS Eligible Clinicians for Payment
Adjustment
Payment adjustment is at TIN/NPI level
•
Exclude TIN/NPIs that meet exclusion criteria
•
– Newly enrolled
– Qualifying APM participant (QP)
– Partial QP
– Low volume threshold
Pull the corresponding CPS score
•
– See slide 48 for special cases
Use CPS score for budget neutrality
•
45
ADVERTISEMENT
0 votes
Related Articles
Related forms
Related Categories
Parent category: Medical
 1
1 2
2 3
3 4
4 5
5 6
6 7
7 8
8 9
9 10
10 11
11 12
12 13
13 14
14 15
15 16
16 17
17 18
18 19
19 20
20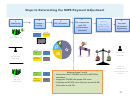 21
21 22
22 23
23 24
24 25
25 26
26 27
27 28
28 29
29 30
30 31
31 32
32 33
33 34
34 35
35 36
36 37
37 38
38 39
39 40
40 41
41 42
42 43
43 44
44 45
45 46
46 47
47 48
48 49
49 50
50